What's Killing Americans and Making Them Sick: IATROGENIC ILLNESS
Focus on how America can close the gap on preventable deaths. From hospital-acquired infections to drug interactions, we must reform healthcare to reduce treatment-related complications.
Iatrogenic illness refers to health complications that arise as a direct consequence of medical treatments and diagnostic procedures. Unlike medical errors, these conditions occur even when care is delivered correctly and according to the best practices. Iatrogenic effects can range from mild to severe and are inherent risks associated with medical interventions designed to diagnose, treat, or prevent disease.
Unlike medical errors, which are preventable by following known protocols, iatrogenic illness is considered to include unpreventable sequelae due to exposure to medical care, procedures, and pharmaceuticals.
Types of Iatrogenic Illness
Hospital-acquired infections. Infections can arise in various healthcare settings and are significant contributors to patient morbidity and mortality, often complicating the course of treatment and extending hospital stays. These infections can be classified into several types, including surgical site infections, bloodstream infections, urinary tract infections from catheters, and respiratory infections from ventilators. Factors contributing to the risk of infection include the duration and type of medical procedures, the sterility of the environment, and the patient's own immune system status.
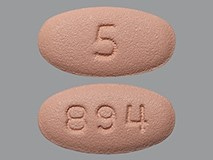
Pharmacological: Adverse drug reactions (ADRs) are the most common type of iatrogenic illness. These reactions can occur due to drug interactions, dosing errors, or as an expected side effect of necessary medication. For example, anticoagulants necessary for preventing thrombosis can increase the risk of bleeding. Some are related to memory issues due to microstrokes, which are hard to detect and differentiate from Alzheimer’s disease in the elderly.
Adverse drug reactions are a significant source of hospital admissions and are estimated to be the fourth leading cause of death in the U.S., with over 100,000 deaths annually. According to the FDA, studies indicate that 6.7% of hospitalized patients have a serious adverse drug reaction with a fatality rate of 0.32%. If these estimates are correct, then there are more than 2,216,000 serious ADRs in hospitalized patients, causing over 106,000 deaths annually.
Surgery is injury. Postoperative complications such as infections, organ dysfunction, or anesthesia-related problems. Even with flawless surgical technique, inherent risks remain due to the body's response to surgical trauma.
Diagnostic complications add to the morbidity and mortality. Invasive diagnostic procedures, such as biopsies or endoscopies, can lead to complications like bleeding, infection, or perforation of organs.
Radiation-Induced illnesses are considered risks worth taking in some cases. Treatments involving radiation, such as those for cancer, can also lead to acute and chronic effects on healthy tissues and organs. Radiation dermatitis occurs in up to 95% of patients receiving radiation therapy and can range from mild skin erythema to severe ulceration.
Vaccine-related adverse events are most frequently unacknowledged or denied. The public health messaging on vaccine safety has created a taboo around real, and not rare, issues from childhood and adult vaccinations. This must be reversed.
Psychological Trauma is an Iatrogenic illness and includes physician burn-out. Just having a series of bad outcomes in the hands of inattentive physicians focused mostly on prescribing drugs to treat symptoms will harm the patient-doctor relationship. This can cause trauma in both physicians and patients.
Chemotherapy-induced neuropathy is a debilitating side effect affecting approximately 30-40% of chemotherapy patients, characterized by nerve pain and sensory loss.
Surgical complications are diverse in nature. Despite sterile techniques and prophylactic antibiotics, Post-Surgical Infections affect about 2-5% of patients undergoing inpatient surgeries in the U.S. each year. Surgical complications account for significant morbidity, with, for example, deep vein thrombosis occurring in up to 80% of patients not receiving proper prophylactic treatment post-operatively.
The Costs
Iatrogenic illnesses are a substantial public health concern, with measurable impacts across various dimensions of healthcare. Accurately quantifying these impacts is essential for informing targeted interventions and policies. Adverse drug reactions alone are responsible for over 100,000 deaths annually in the U.S., making them one of the top causes of death related to medical treatment. Furthermore, surgical complications contribute to prolonged hospital stays for 15% of patients undergoing procedures, significantly increasing healthcare costs and affecting patient quality of life.
The financial implications of iatrogenic illnesses are profound. It is estimated that these conditions cost the U.S. healthcare system billions of dollars annually. These costs arise from additional medical treatments, extended hospital stays, emergency department visits, and increased use of healthcare resources. For example, the additional care required to manage postoperative infections or complications from medication errors adds a considerable financial burden both to healthcare systems and to patients through out-of-pocket expenses.
Iatrogenic Illness is Personal, and in Many Cases, Preventable
Beyond the statistics and economic costs, the personal impact of iatrogenic illnesses on patients and their families is profound and often devastating. Patients may experience prolonged pain and suffering, a decrease in quality of life, and significant emotional distress. Personal stories, such as a patient who suffered chronic pain after a surgical complication or a family that lost a loved one due to a diagnostic error, put a human face on the statistics and underscore the critical need for improvements in patient safety.
Chasing down an elusive diagnosis via differential diagnoses involving specialists not only leads to increases in the cost of healthcare but is also disruptive to personal lives, work productivity, and to family members of the elderly. See, for example, our article on memory loss attributed to apaxiban, a novel anticoagulant given to millions of people hospitalized for COVID-19. In the elderly, the symptoms may be similar to age-related dementia. In younger COVID-19 survivors, the symptoms may be significant contributor to post-COVID-19 brain fog.
Understanding the full scope of the impact of iatrogenic illnesses requires a comprehensive approach that considers these statistical, economic, and personal dimensions, and a willingness to face possibilities as unpalatable to the medical community or pharmaceutical industry as they may be.
Admitting there is a problem is the first step and is a crucial driver for policy change and healthcare practice improvements, aiming to reduce the incidence of these harmful outcomes.
Prevention and Mitigation Strategies
Education and Training
Enhancing education and training for healthcare professionals and patients is fundamental to preventing iatrogenic illnesses. Continuous professional development programs that focus on the latest treatment protocols, medication management, and diagnostic techniques can reduce errors significantly. Simulation-based training has proven particularly effective in preparing teams for high-risk scenarios without endangering patients. Additionally, education should extend to patients, particularly in managing their medication regimens and understanding potential side effects, to empower them as active participants in their own care.
Technology and Innovation
Leveraging technology can significantly mitigate the risk of iatrogenic illness. Implementing advanced electronic health records (EHR) systems with machine-learning optimized prediction science support tools can help prevent medication errors in myriad ways, such as alerting providers to potential drug interactions or allergies or learning how to reduce so-called unpreventable iatrogenic illness. Procedural rituals called flight checks can be implemented to make error reduction routine. Moreover, technologies like barcoding for medication administration ensure that the right patient receives the right dose of the correct medication at the appropriate time. Surgical innovations, such as real-time imaging and robotics, can enhance precision in operations, reducing the risk of procedural complications.
Incentive-Based Policies Are the Answer
Positively reinforcing policies and regulations are crucial to fostering an environment that prioritizes patient safety and reduces the risk of iatrogenic illness with negativity. This includes policies that encourage and reward adherence to safety protocols, regular benchmark incentives for tracked rates of outcomes of practices, and transparently including patients in the learning and detection process. Regulation should require transparent and objective reporting systems for errors and near-misses, which are essential for continuous learning and improvement - with built-in positive reinforcement for proper use and implementation. Penalty-based policies will never encourage a team-based approach to care can enhance communication and coordination among healthcare providers, reducing the risk of errors arising from miscommunication, fear of reprisal, and fragmented care.
Cultural Shift in Healthcare
Modern versions of the Hippocratic Oath no longer include “First, Do No Harm”. Instead, they read quite differently:
“By all that I hold highest, I promise my patients competence, integrity, candor, personal commitment to their best interest, compassion, and absolute discretion, and confidentiality within the law.
I shall do by my patients as I would be done by; shall obtain consultation whenever I or they desire; shall include them to the extent they wish in all important decisions; and shall minimize suffering whenever a cure cannot be obtained, understanding that a dignified death is an important goal in everyone’s life.
I shall try to establish a friendly relationship with my patients and shall accept each one in a nonjudgmental manner, appreciating the validity and worth of different value systems and according to each person a full measure of human dignity.
I shall charge only for my professional services and shall not profit financially in any other way as a result of the advice and care I render my patients.
I shall provide advice and encouragement for my patients in their efforts to sustain their own health.
I shall work with my profession to improve the quality of medical care and to improve the public health, but I shall not let any lesser public or professional consideration interfere with my primary commitment to provide the best and most appropriate care available to each of my patients.
To the extent that I live by these precepts, I shall be a worthy physician.”
Source: Bulger, R. A dialogue with Hippocrates and Griff T. Ross, M.D. In Bulger R, ed. In Search of the Modern Hippocrates. Iowa City: University of Iowa City Press; 1987:25
That’s nice, but where is “Do No Harm?”
Promoting a culture of safety within healthcare organizations is essential. This involves creating an environment where healthcare workers feel safe reporting mistakes and are encouraged to learn from them, rather than fear punishment. Such a culture supports open communication and continuous improvement, critical components for reducing errors. Leadership commitment at all levels is necessary to drive these cultural changes, from executive boards to clinical leaders, underscoring the importance of patient safety as a core value of healthcare delivery.
It does not include teaching medical students that certain losses, while regrettable, are acceptable.
Improved strategies for prevention and mitigation require integrated efforts across the healthcare ecosystem are needed. By addressing the root messaging in medical education and educational needs, utilizing technological advances, enforcing supportive policies, and cultivating a safety-oriented culture, the healthcare system can significantly reduce the occurrence and impact of iatrogenic illnesses. Each strategy can reduce the likelihood of harm to patients and also contribute to a more resilient and effective healthcare system.
We call on allopathic medical professional societies to undertake soul-searching, ask themselves whether paternalism has served the public well, and identify means of implementing programs that use positive reinforcement.
The call for allopathic medical professional societies to introspect on the effectiveness of paternalistic practices opens up an avenue to reimagine patient safety measures. By shifting towards a model of collaborative care, these societies can foster more inclusive and effective healthcare practices. Here are expanded ideas and new strategies for implementing positive reinforcement programs:
Hand-Washing
- Develop a digital tracking system with sensors in sinks that record hand hygiene compliance and provide real-time feedback to healthcare workers. Introduce gamification in the workplace where teams can earn points for compliance, which can be redeemed for rewards or recognition at staff meetings.
Reducing Polypharmacy
- Implement smart pharmacy systems that automatically flag potential drug interactions at the point of prescribing and dispensing - and at home. Establish annual comprehensive medication reviews conducted virtually, where pharmacists can consult with patients to optimize their medication regimens, thereby reducing unnecessary polypharmacy.
Better Sanitation
- Introduce unannounced spot checks combined with clearly stated performance-based financial rewards for custodial staff who maintain exemplary sanitation standards in rooms in their charge. Utilize UV light scanning technology to detect areas that may have been missed during cleaning, ensuring thorough sanitation, and UV-C sanitation in empty rooms.
Flight Check Procedures
- Adopt aviation-style checklists and pre-procedure time-outs for all surgical and high-risk medical procedures. These checklists should be digital and interactive, ensuring all steps are completed and recorded. Implement a system where team members are encouraged and rewarded for actively participating in these checks.
Encouraging Reporting of Near-Misses
- Create a non-punitive system for reporting and analyzing near-misses, also similar to the aviation industry's safety reporting systems. Offer incentives for staff who report these incidents, which provide crucial learning opportunities and can prevent future errors.
Patient and Patient Family Involvement
- Patient and patient family involvement in double-checking (product insert review, ways to ping physicians that do not involve office visits, say, via web messaging or email).
- Enhance patient and family involvement by providing accessible, easy-to-understand product inserts and online resources that can be accessed through QR codes. Develop platforms for secure web messaging or email communications where patients can pose questions or confirm understanding about their treatments without needing an office visit. Introduce a ‘patient safety advocate’ role in healthcare settings, where designated staff can help patients and families navigate their care and double-check critical elements of their treatment plans.
Involvement of All Staff in Safety Protocols
- Extend training and responsibility for patient safety protocols beyond healthcare providers to include all hospital staff. Everyone from administrators to cafeteria workers should understand how their role impacts patient safety, and be involved via positive reinforcing incentive structures in ongoing education and improvement initiatives.
By adopting these strategies, medical professional societies can lead a shift towards a more preventive, inclusive, and patient-centered approach to healthcare. These changes not only enhance patient safety but also empower all participants in the healthcare system to contribute actively to reducing iatrogenic risks.
The Payoffs
Implementing the above strategies could lead to substantial cost savings in healthcare, both in terms of human costs and economic expenditures. By enhancing hand hygiene through monitoring and gamification, healthcare facilities could see a significant reduction in hospital-acquired infections, which are among the costliest medical errors, averaging about $20,000 to $25,000 per incident. Reducing polypharmacy through automated systems could decrease adverse drug reactions, which are reported to result in over 1.3 million emergency room visits each year, thereby lowering emergency care costs and reducing the burden on healthcare resources.
Further, adopting aviation-style checklists for surgical and procedural interventions could lead to fewer surgical mistakes and complications, potentially saving up to $1.5 billion annually in the U.S. alone, a figure derived from the estimated costs of surgical errors. Enhanced sanitation and reward programs for custodial staff could also prevent outbreaks of infections like C. difficile, which are expensive to treat and lead to extended hospital stays.
Engaging patients and families more directly in the care process, especially through digital communication tools, would not only improve patient satisfaction and safety but could also reduce the frequency of unnecessary office visits and hospital readmissions, a significant cost driver in healthcare. Additionally, encouraging the reporting of near-misses and adopting a non-punitive approach to errors could further enhance learning and prevention, helping to avert costly future errors.
Collectively, these proactive measures could save thousands of lives each year, dramatically reduce morbidity associated with medical treatments, and potentially save the healthcare system billions of dollars annually by preempting costly medical complications and fostering a more efficient, safety-focused healthcare environment. These savings could then be redirected towards improving quality of care, funding more comprehensive patient education programs, and investing in advanced healthcare technologies, which in turn would feed a cycle of continuous improvement and cost reduction.
Of course, that’s not where savings go in healthcare, but that’s a topic for another series or policy paper.
In our next article in this series, we will explore Preventing and Reversing Diabetes.








Dr: “Vaccines are safe”
Pt: “How do you know?”
Dr: “There are no reported injuries”
Pt: “I have a vaccine injury”
Dr: “No you don’t, vaccines are safe”
Great read. At age 57 and my dad dying from Prostate Cancer Metastasis after 10 years, I was flagged for a UK NHS PSA screening test. 7.2 so next step MRI. I refused Galidium contrast "dye", but they found a dark patch anomaly. Next step biopsy they said. No Thanks. Paid £415 for a private Stockholm 3 test yesterday, results due 2-3 weeks. If anything risky shows, will go down the Tippens Fenbendazole and Ivermectin route. No slash and burn oncology for me.