What's Killing Americans and Making Them Sick: DIABETES
Article 3 in the Popular Rationalism series "What's Killing Americans and Making Them Sick"
Diabetes, the eighth leading cause of death in the United States, is a significant public health concern, with profound impacts on morbidity, mortality, and the overall well-being of affected individuals. The disease's complex nature leads to a myriad of health complications that place burdens on society through lost productivity, disabilities, and early deaths.
Comorbidities and Health Complications of Diabetes
Cardiovascular Disease. Diabetes significantly increases the risk of cardiovascular disease, including heart attacks and strokes. According to the American Diabetes Association (ADA), adults with diabetes are 2 to 4 times more likely to develop heart disease than those without diabetes. This risk stems from diabetes-related factors, such as hypoglycemia (low blood sugar), insulin resistance, and lipid abnormalities, which contribute to atherosclerosis and cardiovascular events.
Kidney Disease. Diabetic nephropathy, or kidney damage resulting from high blood glucose levels, affects 1 in 3 adults with diabetes. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reports that diabetes is the leading cause of kidney failure, accounting for nearly 40% of new cases in the United States each year.
Vision Loss. Diabetic retinopathy is another serious complication, affecting up to 40% of individuals with diabetes. This condition occurs when high blood glucose levels damage the blood vessels in the retina, leading to vision impairment or blindness. Additionally, diabetes increases the risk of other eye conditions, such as cataracts and glaucoma.
Neuropathy. Diabetic neuropathy, characterized by nerve damage due to high blood glucose levels, affects 50% of individuals with diabetes. This condition can lead to symptoms such as numbness, tingling, and pain, particularly in the extremities. Neuropathy also increases the risk of foot ulcers and infections, potentially leading to amputations.
Lost Work and Disabilities
Productivity Loss. The American Diabetes Association estimates that diabetes contributes to nearly $90 billion in lost productivity annually. This figure includes absenteeism, reduced work capacity due to diabetes-related health complications, and premature deaths.
Disabilities. Diabetes-related complications can also lead to permanent disabilities. For example, neuropathy and foot ulcers may result in mobility impairments, while vision loss and kidney failure can lead to significant long-term disabilities that impact an individual's ability to work and maintain daily activities.
Diabetes-Related Early Deaths
Premature Mortality. The Centers for Disease Control and Prevention (CDC) reports that diabetes is the 8th leading cause of death in the United States, contributing to approximately 100,000 deaths annually. This figure includes direct deaths from diabetes-related complications and deaths where diabetes was an underlying or contributing factor.
Reduced Life Expectancy. Individuals with diabetes are at risk of reduced life expectancy due to the disease's cumulative impact on health. The CDC estimates that diabetes can shorten life expectancy by up to 10 years, particularly in individuals with poorly managed blood glucose levels or those experiencing severe diabetes-related complications.
The morbidity and mortality burden of diabetes in the United States is profound, with the disease leading to numerous comorbidities, lost productivity, disabilities, and early deaths. This emphasizes the importance of comprehensive prevention and management strategies to reduce the impact of diabetes on individuals and society.
The Pathophysiology of Diabetes
The pathophysiology of diabetes varies between Type 1 and Type 2 diabetes, but both conditions ultimately lead to elevated blood glucose levels and require comprehensive management strategies. The emergence of new therapies, such as intranasal insulin, which may serve both as preventative and treatment options, offers innovative solutions to complement traditional approaches, highlighting the need for both medical and lifestyle interventions in diabetes management.
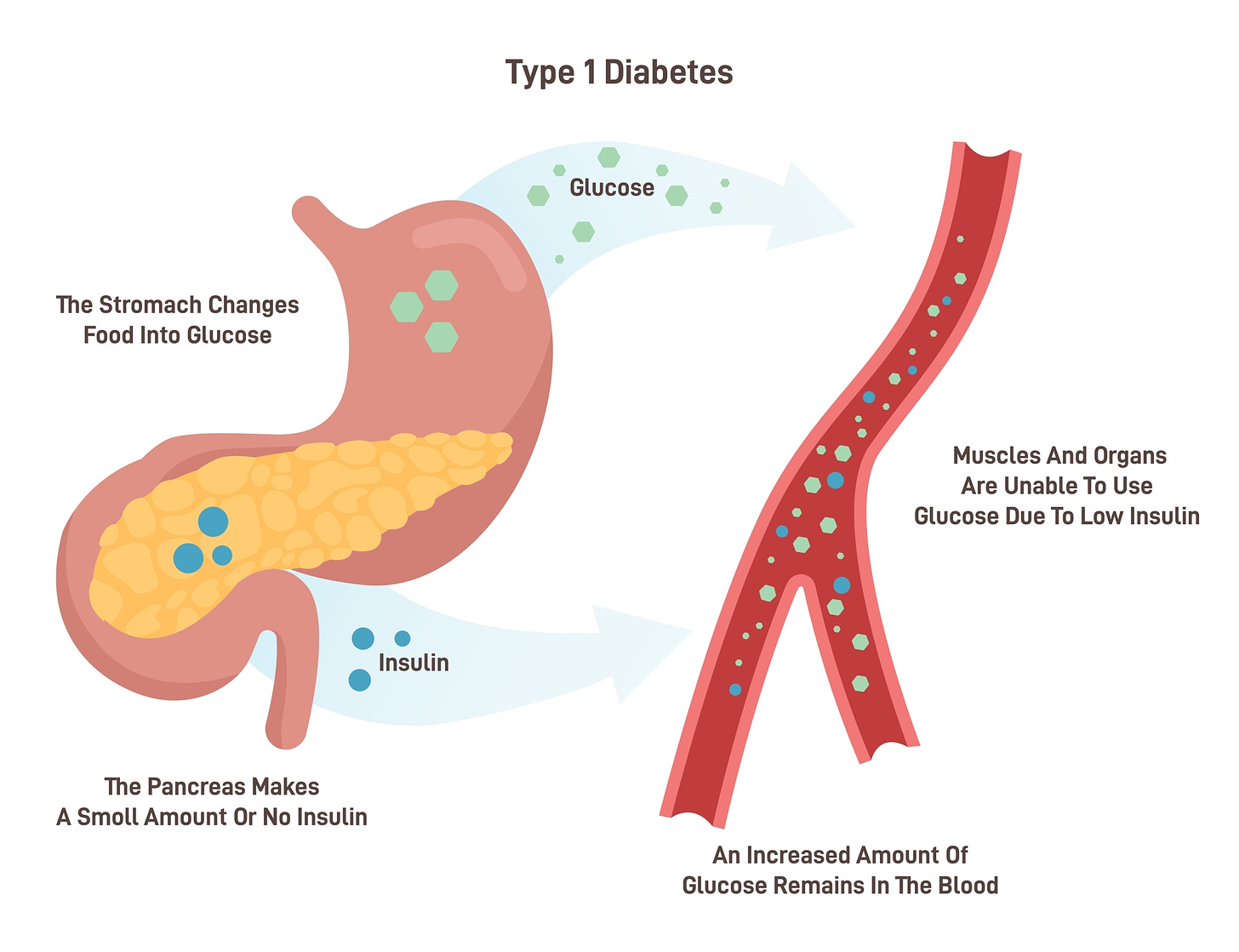
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the body's immune system attacks and destroys pancreatic beta cells, resulting in an inability to produce insulin. Without insulin, glucose cannot enter the cells, leading to elevated blood sugar levels and associated symptoms such as frequent urination, excessive thirst, and fatigue.
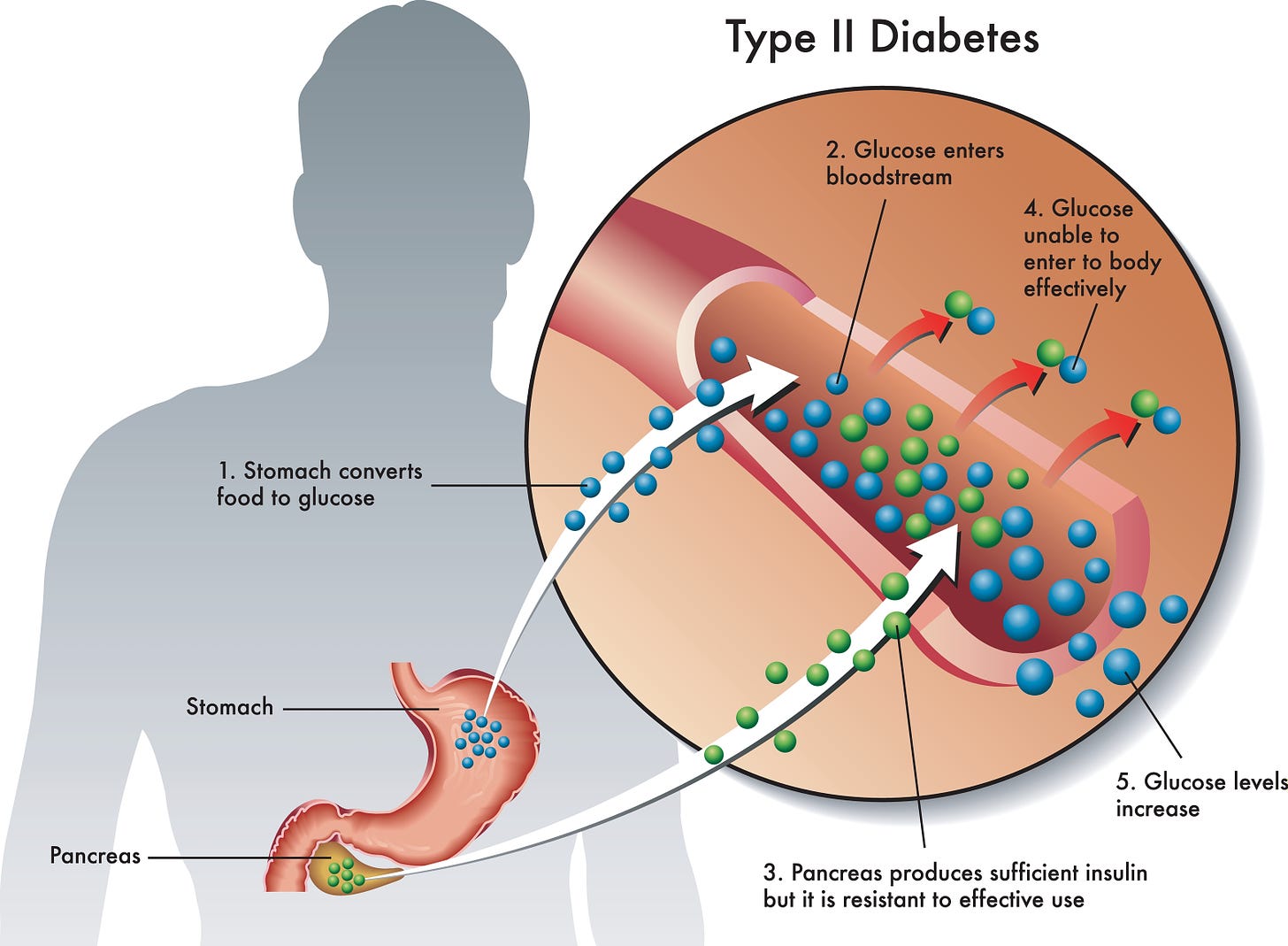
Type 2 Diabetes
Type 2 diabetes is a progressive metabolic disorder characterized by insulin resistance, where the body's cells become less responsive to insulin. Initially, the pancreas compensates by producing more insulin, but over time, beta-cell function diminishes, leading to elevated blood glucose levels. The progression from insulin resistance to full-blown diabetes is influenced by several factors:
Diet and Lifestyle. Poor dietary choices, particularly diets high in refined carbohydrates and sugars, contribute to insulin resistance. Sedentary lifestyles further exacerbate this condition by reducing the body's ability to utilize glucose effectively.
Adipose Tissue and Inflammation. Excessive visceral fat can secrete pro-inflammatory cytokines that impair insulin sensitivity and further strain pancreatic beta cells.
Genetic Factors. Genetic predispositions can also play a role, influencing an individual's susceptibility to insulin resistance and the eventual dysfunction of beta cells.
Intranasal (IN) Insulin as a Potential Therapy
Intranasal insulin is emerging as a promising therapy, particularly for individuals with early-stage Type 2 diabetes. This form of insulin delivery bypasses the digestive system and enters the bloodstream directly through the nasal mucosa, leading to a rapid and stable insulin response. Additionally, intranasal insulin has shown potential cognitive benefits, making it a dual-purpose therapy for managing both diabetes and preventing cognitive decline, which is often associated with diabetes and insulin resistance. IN insulin has the potential for stabilizing blood glucose levels in pre-diabetic individuals, strengthening its position as both a treatment and preventive measure.
Reversal Strategies for Type 2 Diabetes
Low-Calorie Diets. Low-calorie diets have been shown to lead to substantial weight loss and improve insulin sensitivity, contributing to the reversal of Type 2 diabetes. These diets often focus on nutrient-dense foods while limiting caloric intake, thereby reducing blood glucose levels and the strain on pancreatic beta cells.
Low-Carbohydrate and Ketogenic Diets. Diets that restrict carbohydrates, particularly ketogenic diets, can induce a state of ketosis where the body uses fat as its primary energy source. This helps reduce blood glucose levels and\ also improves insulin sensitivity and beta-cell function over time. These dietary approaches can also lead to significant weight loss, further aiding in diabetes reversal.
Exercise Programs. Regular physical activity is essential for managing and reversing Type 2 diabetes. Aerobic exercises, such as walking, swimming, and cycling, can lower blood glucose levels by improving insulin sensitivity and glucose uptake in muscle cells. Resistance training, such as weightlifting, can also increase muscle mass, further enhancing glucose metabolism.
Recommended Programs. A combination of aerobic exercise and light resistance training, at least 150 minutes per week, is recommended for optimal metabolic health. This regimen can help reduce blood glucose levels, promote weight loss, and improve overall well-being, contributing to diabetes reversal.
Managing Blood Glucose Levels with Intranasal Insulin as a Supportive Therapy
Intranasal insulin offers a rapid and stable insulin response, helping stabilize blood glucose levels in individuals with Type 2 diabetes. This therapy can support lifestyle interventions and other medical treatments by reducing the need for additional medications and helping manage blood glucose fluctuations.
Case Studies and Research
DiRECT Trial
The Diabetes Remission Clinical Trial (DiRECT), carried out at Newcastle University , demonstrated that intensive lifestyle interventions, including a low-calorie diet and weight management support, led to remission in nearly half of the participants after one year, without the use of diabetes medications. It was the first to show that remission from type 2 diabetes is possible through a dietary intervention in primary care, with almost half (46%) of people in remission at one year, and 36% at two years.
The Look AHEAD Study
The Look AHEAD study showed that intensive lifestyle interventions led to significant reductions in glucose levels, with some participants achieving partial or complete diabetes remission. This study underscores the potential for lifestyle changes to effectively reverse Type 2 diabetes.
The Look AHEAD (Action for Health in Diabetes) study aimed to investigate whether intensive lifestyle interventions, including weight loss and increased physical activity, could improve cardiovascular outcomes in individuals with Type 2 diabetes.
The study enrolled over 5,000 overweight or obese adults with Type 2 diabetes across 16 clinical sites in the United States.
Participants were randomly assigned to one of two groups:
- Intensive Lifestyle Intervention (ILI): This group received a comprehensive program promoting weight loss through dietary changes, increased physical activity, and behavioral therapy, including individual and group counseling.
- Diabetes Support and Education (DSE): This group received standard diabetes education and support, including information on managing the disease through diet, exercise, and medication adherence.
The study began in 2001 and followed participants for a median of 10 years, collecting data on health outcomes.
Cardiovascular Events. The primary endpoint was to compare the rates of cardiovascular events, including heart attacks, strokes, and cardiovascular deaths, between the two groups. The study found no significant difference in cardiovascular event rates between the ILI and DSE groups.
Weight Loss. The ILI group experienced greater weight loss than the DSE group, losing an average of 8.6% of their initial body weight at one year, compared to 0.7% for the DSE group. This weight loss was sustained over the long term, with the ILI group maintaining a greater loss.
Other Health Outcomes. The ILI group saw other health benefits, including improved glucose control, reduced need for diabetes medications, and a lower risk of developing sleep apnea. Improvements in mobility, physical functioning, and quality of life were also noted.
The Look AHEAD study showed that intensive lifestyle interventions can lead to significant weight loss and improvements in health outcomes for individuals with Type 2 diabetes. The study highlighted the benefits of comprehensive lifestyle changes in managing diabetes and improving overall health and quality of life.
Reversing Type 2 diabetes is possible through a combination of dietary changes, regular exercise, and medical interventions. Low-calorie and low-carbohydrate diets, along with regular exercise programs, can improve insulin sensitivity and promote weight loss, contributing to diabetes reversal. Additionally, treatments such as bariatric surgery and intranasal insulin offer further support, stabilizing blood glucose levels and enhancing metabolic health. These strategies, backed by clinical research, provide a comprehensive approach to reversing Type 2 diabetes and improving long-term health outcomes.
Challenging the Healthcare Industry's Economic Models
Treatment-Centered Profit Motives in Healthcare
The current healthcare industry's focus on treating symptoms rather than addressing root causes exacts an obvious cost: failure to reverse diabetes. This model benefits economically from managing chronic diseases such as diabetes with a steady stream of medications and treatments but fails to address the underlying issues that lead to these conditions.
The pharmaceutical and medical device industries profit significantly from a treatment-centered approach, developing new medications, insulin pumps, and continuous glucose monitors that generate substantial revenue. This dynamic discourages investment in prevention and reversal strategies, perpetuating the cycle of chronic disease management.
Preventive and Reversal Strategies in Sustainable Healthcare Systems
Healthcare systems that prioritize preventive and reversal strategies should be recognized for the long-term benefits of these approaches for both patients and the healthcare system. This includes comprehensive coverage for lifestyle interventions, such as dietary counseling, exercise programs, and mental health support, which can reduce the need for long-term medications and medical devices.
Comprehensive Care Models
Care models that integrate preventive and reversal strategies into primary healthcare, should be promoted, ensuring that individuals receive comprehensive care tailored to their needs. This includes regular screenings, risk assessments, and lifestyle interventions that can delay or prevent the onset of Type 2 diabetes, as well as supportive medical treatments like intranasal insulin for effective management and reversal.
Economic Benefits of Prevention and Reversal
Reduced Long-Term Costs. Outline how investing in prevention and reversal strategies can reduce the long-term costs associated with managing chronic conditions like diabetes. These approaches decrease the burden on healthcare systems, reducing the need for ongoing treatment and allowing resources to be allocated to other areas.
Supporting Sustainable Wellness. A focus on prevention and reversal strategies fosters sustainable wellness, reducing the prevalence of diabetes and its associated complications. This approach benefits individuals, communities, and healthcare systems alike, promoting a healthier future.
Challenging the healthcare industry's economic models requires a shift from treatment-centered approaches to prevention and reversal strategies. This paradigm benefits individual patients and supports sustainable wellness at a societal level. By integrating comprehensive care models and investing in preventive measures, healthcare systems can reduce long-term costs and improve outcomes for individuals with diabetes, creating a healthier future for all.
Policy and Practice Reforms
Integrating Comprehensive Diabetes Management into Primary Healthcare Systems
Holistic Care Models. Integrate risk assessments, and customized early prevention-focused intervention plans for diabetes management directly into primary care practices. This integration ensures that diabetes management is not isolated but part of general health maintenance.
Lifestyle Modification Coaches. Form multidisciplinary teams including endocrinologists, dietitians, diabetes educators, and mental health professionals. These teams collaborate to provide holistic care tailored to individual patient needs, from medical management to lifestyle counseling.
Chronic Care Management Programs. Implement chronic care management programs that offer structured and continuous care for diabetes patients. These programs include regular monitoring and adjustments in treatment plans based on patient progress and feedback.
Enhancing Diabetes Education Among Healthcare Providers
Specialized Training. Implement mandatory training programs for healthcare providers, focusing on the latest diabetes treatment protocols, technological advancements in patient care, and patient-centered communication skills.
Continuing Education. Encourage ongoing education through workshops, seminars, and online courses to keep medical staff updated on the evolving landscape of diabetes research and treatment strategies.
Educating Patients
Diabetes Self-Management Education (DSME). Provide comprehensive DSME programs that empower patients to manage their diabetes effectively. These programs cover nutrition management, the importance of physical activity, blood glucose monitoring, and the correct use of medications.
Community-Based Education Initiatives. Launch community outreach programs to raise awareness about diabetes prevention and management. These include free screening days, informational talks, and cooking classes focused on healthy eating.
Insurance Reforms to Ensure Coverage for Preventive Care and Treatments
Preventive Services. Include comprehensive coverage for preventive services such as routine risk assessment and regular screenings for high-risk individuals, and promote lifestyle interventions that prevent complications related to diabetes. Tie insurance discounts to lifestyle changes that reduce the risk of diabetes.
Coverage for Diabetes Management Tools. All health insurance plans must include advanced diabetes management tools like lifestyle self-management diaries, CGMs (Continuous Glucose Monitors) and insulin pumps without cumbersome pre-approvals or prohibitive co-pays.
Economic Incentives for Healthy Choices
Subsidies for Healthy, Organic Foods. Provide subsidies for low-income families to access healthy foods, helping to manage or prevent diabetes. This includes vouchers redeemable at local farmers’ markets or discounts on whole-food-based meal kits.
Tax Incentives. Introduce tax incentives for businesses that provide wellness programs, healthy eating options, and exercise facilities to their employees.
Incentivizing Physical Activity. Support initiatives that provide financial or other rewards for documented physical activity, such as discounted gym memberships or fitness-related equipment through health insurance plans.
Addressing the diabetes epidemic requires coordinated, sweeping efforts across healthcare systems, educational bodies, and insurance sectors. By implementing comprehensive care models, enhancing educational efforts, and reforming insurance policies to support preventive care and effective diabetes management, significant strides can be made in improving outcomes for individuals with diabetes. These reforms will facilitate better management of diabetes and foster a healthcare environment that supports sustainable, health-promoting practices across the population.
Prioritizing Prevention and Reversal of Diabetes in Community and Society
Community Gardens and Local Markets. Promote the establishment of community gardens and local markets that provide access to fresh, healthy foods. These initiatives help combat food deserts and encourage dietary changes that can prevent the onset of Type 2 diabetes.
Fitness Programs. Implement community-led fitness programs, such as free yoga classes in the park, community sports leagues, and walking clubs that make physical activity accessible and enjoyable for all age groups.
Workplace Wellness Programs. Encourage workplaces to introduce wellness programs that include regular health screenings, workshops on nutrition and exercise, and incentives for employees to engage in healthy behaviors. These programs can significantly reduce the incidence of Type 2 diabetes among the working population.
Leveraging Educational Institutions
Curriculum Integration. Advocacy is needed for the integration of comprehensive health education into school curriculums, focusing on nutrition, the importance of physical activity, and the science of diabetes prevention.
Healthy School Meals. Work with schools to improve the nutritional quality of meals served, ensuring they are low in sugar and high in fiber, to help instill healthy eating habits from a young age.
Higher Education. Support colleges and universities in developing programs that encourage research on diabetes prevention and the development of new public health strategies focused on lifestyle choices and avoiding causes of autoimmunity (e.g., aluminum-containing vaccines).
Engaging Places of Worship. Places of worship often have the trust and attention of large segments of the community. Encourage these institutions to set up health ministries that can deliver educational sessions on diabetes prevention and support congregants in maintaining healthy lifestyles.
Public Awareness Campaigns (Television and Radio). Use these media to run public service announcements that educate the public on diabetes risks and prevention strategies.
Social Media Campaigns. Leverage social media's power to promote healthy lifestyles and create viral challenges that encourage physical activity and healthy eating.
Policy Advocacy for Preventive Measures (Support for Preventive Legislation)
Advocacy is needed for policies that support preventive health measures, such as taxes on sugary drinks, subsidies for gym memberships, and funding for public health campaigns focused on diabetes prevention.
Urban Planning for Health. Promote urban planning policies that prioritize pedestrian-friendly infrastructure, ample green spaces, and public sports facilities to encourage a physically active lifestyle. Encourage easy access to healthy food vendors.
Intranasal Insulin as a Treatment Option
Direct Insulin Delivery
Intranasal insulin offers an innovative method of insulin delivery with immediate absorption. It bypasses the digestive system and enters the bloodstream directly through the nasal mucosa. This provides a rapid and stable insulin response, helping to regulate blood glucose levels quickly and effectively.
Non-Invasive Delivery. This method is non-invasive, eliminating the need for injections or infusions, which can improve adherence and comfort for individuals with diabetes.
Cognitive Benefits - Protection Against Cognitive Decline. Intranasal insulin has shown promise in improving cognitive function and potentially preventing cognitive decline. This is particularly significant for individuals with diabetes, who are at higher risk of cognitive impairment due to the long-term effects of high blood glucose levels.
Neurological Impacts. The nasal route also allows insulin to directly reach the brain, potentially influencing neurological pathways associated with memory, learning, and mood. This dual-purpose therapy can improve both metabolic and cognitive health.
Potential for Prevention
Intranasal insulin can help stabilize blood glucose levels in pre-diabetic individuals, potentially delaying or preventing the onset of Type 2 diabetes. This form of therapy provides an additional tool for managing glucose levels in conjunction with lifestyle changes, such as diet and exercise.
Inclusion in Health Plans. Advocacy is needed for the inclusion of intranasal insulin in health insurance plans to make this therapy more accessible. Comprehensive coverage can reduce patients' financial burden and improve adherence to treatment.
Reduced Co-Pays. To ensure patients have immediate and affordable access to intranasal insulin, we can propose reducing co-pays and removing pre-approval Regulatory Easing.
Recommendations from FDA and Diabetes Societies. Advocacy is needed to encourage supportive regulatory measures that expedite the adoption of new therapies like intranasal insulin, allowing for faster implementation and wider access. This is particularly important for therapies that offer unique benefits, such as intranasal insulin’s cognitive and metabolic impacts.
Intranasal insulin represents a promising innovation for diabetes management and prevention. It offers rapid and stable insulin delivery and potential cognitive benefits. This therapy's noninvasive nature makes it an appealing option for patients, while its ability to stabilize blood glucose levels can aid in preventing Type 2 diabetes. Ensuring accessibility through insurance coverage and regulatory support is crucial for integrating this therapy into comprehensive diabetes care, ultimately contributing to improved health outcomes and sustainable wellness.
Summing it Up: Prevention and Reversal Over Treatment
Shifting the focus from treatment to prevention and reversal of diabetes requires a societal transformation where every segment of the community is engaged—from schools and workplaces to places of worship and the media. By empowering communities, enhancing educational efforts, and utilizing broad-reaching media, society can significantly reduce the prevalence of diabetes. This approach addresses the health of individuals and enhances community well-being while also reducing the long-term economic burden on the healthcare system. This proactive, preventive strategy ensures that diabetes prevention and reversal are not just healthcare goals but societal priorities.
The traditional healthcare model, often focused on treating symptoms rather than addressing root causes, may indeed prove lucrative for those selling treatments and medications. However, for those on the receiving end—the patients—this approach can cost them far more than just financial resources. It can cost them their health, their quality of life, and in severe cases, even their lives.
Our current healthcare paradigm is effective in managing symptoms and acute crises. However, it often overlooks the long-term strategy of empowering individuals to avoid disease onset through lifestyle and environmental changes and avoiding autoimmune-inducing aluminum of all types.
The case for prioritizing prevention and reversal over treatment is compelling, not only from a health and wellness perspective but also from an economic standpoint. Investing in prevention and reversal strategies, such as community-based programs, education in schools, and widespread public health campaigns, holds the potential to reduce the vast expenditures associated with managing chronic diseases. These initiatives encourage a healthier, more informed population, reducing the overall dependence on pharmaceutical solutions and intensive medical care.
Moreover, the focus on sustainable health practices that prevent illness aligns with a broader view of well-being that encompasses physical health, mental health, and environmental health, promoting a more holistic approach to living well. This perspective underscores the importance of societal involvement—from educational systems to media outlets and local community leadership—to foster an environment where healthy choices are accessible and encouraged.
Ultimately, by emphasizing prevention and reversal, we challenge the existing healthcare economic models that benefit from perpetual treatment and become advocates for a paradigm where the true value is placed on genuine, sustainable wellness. This approach, while perhaps less profitable for the healthcare industry, promises a richer, healthier life for individuals, proving that the greatest wealth is indeed health.
An Urgent Call to Action for Prevention and Reversal
The diabetes epidemic in the United States is a growing public health crisis, contributing to substantial morbidity, mortality, and economic burdens. Now is the time to take decisive action to address this issue holistically, integrating a broad range of strategies that encompass prevention, treatment, and societal change. This comprehensive approach can save lives, improve health outcomes, and alleviate the economic strain of managing chronic illnesses.
Supporting Mental Health and Behavioral Well-Being
Diabetes management places a significant psychological burden on patients, leading to stress, anxiety, and depression. We need to offer comprehensive mental health support, including therapy, support groups, and mindfulness programs, to help individuals manage their condition's emotional impact.
Addressing the Needs of an Aging Population
As diabetes prevalence increases with age, we must consider the unique challenges faced by older adults. Comprehensive care plans should address cognitive decline, reduced mobility, and comorbidities that exacerbate diabetes symptoms, ensuring a higher quality of life for aging individuals with diabetes.
Tackling Socioeconomic Factors
Socioeconomic status plays a critical role in diabetes risk and outcomes. We must address the disparities created by income level, education, and access to healthy foods and exercise opportunities. This includes implementing policies and programs that ensure equitable access to resources for all communities.
Recognizing Cultural Factors
Cultural attitudes toward food, exercise, and health significantly impact diabetes prevention and management. Interventions tailored to specific cultural communities, including culturally relevant dietary education and exercise programs, are essential for effective diabetes care across diverse populations.
Leveraging Technological Innovations
New technologies, such as applications that encourage lifestyle changes, prompt blood sugar level checks, and improve awareness of the availability of intranasal insulin, offer promising advancements in diabetes care. We must support the development and adoption of these innovations to improve treatment options, enhance management, and reduce the burden of diabetes.
Public Health Policies
Government-funded health campaigns, regulations on food labeling and marketing, and policies supporting diabetes research are crucial for comprehensive diabetes prevention. Public health initiatives can educate the public, promote healthier lifestyles, and support the development of new treatments. Increasing public awareness of the role of aluminum as a root causal factor in autoimmunity will be an essential part of public health messaging.
CALL TO ACTION
The time for action is now. We must address the diabetes epidemic with a comprehensive, integrated approach that spans healthcare access, mental health support, socioeconomic factors, cultural attitudes, technological innovations, and public health policies. By doing so, we can reduce the prevalence of diabetes, improve health outcomes, and alleviate the economic strain on individuals, communities, and the nation. This holistic strategy is essential to creating a healthier future for all.
RELATED





I was diagnosed with T2 diabetes about 30 years ago. My doctor advised me to alter my diet and sent me to a nutritionist. I wasn’t satisfied after a few years and asked him to refer me to a specialist. Big Mistake! All the specialist kept doing was prescribing new and more expensive drugs with lots of side effects. The one that said it wasn’t a weight loss drug but you may lose weight made everything I ate and my cigars taste horrible, no wonder you might lose weight! I went back to my doctor who recommended old generic metformin with a small amount of basal insulin. Unfortunately, he also recommended triglyceride meds and statins because all the literature said that I needed them.
After several years, I dropped the triglyceride meds as I did my own research and a few years later dropped the statins as well. Most people, even diabetics, don’t meet the risk to benefit ratio for those meds, but they automatically prescribe them for diabetes.
I’m now on a modified KETO diet and have cut the metformin in half and dropped the insulin from 35 units to just 15 which I expect to drop soon to 0.
Two books I read recently, Rethinking Diabetes and Life Without Diabetes, opened my eyes to the insanity that has been going on with diabetes research and treatment. It’s almost all for the financial health of big pharma and only tangentially for the physical health of the patient!
Thanks for the opportunity to rant, I feel better now.
Inflammation ….. our bodies hate it