
In the United States, Vaccination Rates Are Associated with Increased Rate of Spread of SARS-CoV-2, But Not How They Should Be
We can debate the details of the analysis, but the persistent and repeated positive association is the opposite of what we should expect if COVID-19 vaccine program reduces transmission and disease.
DEAR READER - DO NOT BE INTIMIDATED BY THE ANALYSIS. PUSH THROUGH AND GET WHAT YOU CAN FROM THIS. - AUTHOR
A while ago, I published a country-level analysis that hinted at the fact that there is a positive correlation between vaccine uptake and SARS-CoV-2 infection. My motivation was that epidemiological evidence was pointing to zero or negative vaccine efficacy, and the balance of evidence pointed to potential disease enhancement from vaccination against coronaviruses and other respiratory viruses.
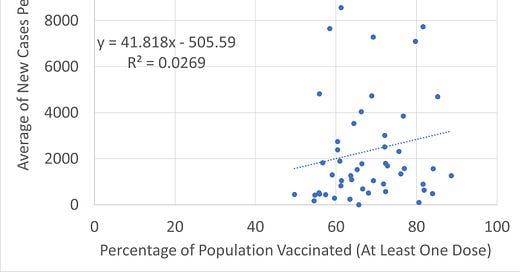
I present here a state-wide analysis (using data from US States) that makes a simple comparison: the percentage of population vaccinated in each state vs. the average number of new cases of COVID-19 diagnoses by state. If vaccines are effective at reducing COVID-19, there should be a negative relationship between vaccination effort and COVID-19 cases. The US State-level data allow yet another test of the hypothesis of disease enhancement due to COVID-19 vaccination.
If vaccines reduce the rate of transmission, or make the symptoms more mild (fewer diagnoses), we would expect a NEGATIVE RELATIONSHIP (literally a negative sign on the value of a parameter that describes the relationship, as in “-2.4”; more vaccination should lead to a stepwise decrement in COVID-19 diagnosis per unit increase in vaccination. The states with the highest vaccination uptake per capita should have the lowest number of new cases.
Analysis 1. New Cases Regressed on Vaccine Uptake, Free Intercept
In the comparison of two variables like vaccine uptake and average weekly new case rate, we can assume that the intercept (y-axis) is zero (zero vaccine uptake, zero cases), or allow the linear model to tell us what the intercept is.
If we allow the intercept to be free, we do not see a negative correlation; in fact, we see a positive, but likely not significant, correlation, but a negative intercept:
Analysis 2. New Cases Regressed on Vaccine Uptake, Fixed Intercept
In the fixed intercept model, the slope is positive, and we see an increase in the R-squared, the measure of the goodness of fit to the model (completely expected). We lose a degree of freedom.
Which model is “correct”?
This is snapshot analysis in a long, dynamic process with likely feedback between the two variables. People in states with higher reported case rates might be more likely accept vaccination as a possible route to safety. The negative intercept may tell us the model is under-specified.
The forced zero intercept model would result in the loss of a degree of freedom in statistical hypothesis testing. There are arguments for and against “ever” using a zero intercept model. (These arguments can be read here). Clearly, there were COVID-19 cases before the vaccines were developed, so a non-zero intercept reflects reality. Given the scatter, however, the estimated intercept parameter estimate is unreliable.
It is noteworthy that the slope parameter is the primary parameter of interest, which is positive, but not statistically significant, in either analysis.
The large amount of scatter (spread) leads to a poor fit of the data to the model, so interpretation of the slope parameter should be considered “hazardous”. But then again, even with the large amount of scatter and free to estimate intercept model is not negative, as would be expected if the vaccination contributed to herd immunity.
The most anyone can say about these data with reliability is that something is causing the expected relationship to fail to manifest. There is certainly no evidence in the all-states level data that vaccination contributes to a reduction in the number of new cases.
Vaccination Coverage and Population Density
When individual variables fail to show expected relationships, other variables might be impacting the analysis. It’s possible that the role of vaccination might look different after other among-state variation in the new case rate is accounted for. In these conditions, a multiple regression analysis is worth exploring.
In our multiple regression analysis, we will specify two predictor variables (X1 and X2) and attempt to derive a model that best describes the relationship between those two variables, and an outcome (dependent variable (Y)).
In the present problem,
X1 = vaccination coverage in each state X1 = {x1,1, x1,2, x1,3… x1,50}
X2 = population density in each state X2 = {x2,1, x2,2, x2,3… x2,50}
Y = average number of new cases per week (current) = {y1,y2,y3…y50}
The equation we seek to derive is a PREDICTED value of Y, so we denote it Y-hat.
Y-hat = predicted average number of new cases per week.
Y-hat = m1x1 + m2x2 + b
where m1 and m2 are the slopes parameters that best fit the model under least squares assumptions, and b is the intercept. In this equation m1x1 means “slope parameter 1 TIMES predictor variable 1”. The following parameters are estimated using methods that minimize overall the error (deviation) in the model across the range of measurements: m1, m2, b). This is all standard linear regression stuff.
The important is that when doing this with X1 = vaccination coverage and X2 = state population density, if vaccination reduces the spread of SARS-CoV-2, the parameter m1 should be negative; i.e., vaccination should reduce the number of new cases.
y-hat =5.355X1 + 3.0427X2 + 1423.59
Written out, this reads
“Predicted average weekly number of cases = 5.3 cases per unit increase in vaccination uptake plus 3.04 additional cases per person per mile plus a constant of 1423”.
The p-value for VaxUptake is not significant, and neither is the overall model.
Unfortunately, though, the m1 parameter is not negative.
In multiple regression, we can also test for an interaction between x1 and x2 (x1 might modify the effect of x2 on y, or vice versa).
The formal model equation is
y-hat=β0+β1x1+β2x2+β1,2x1∗x2y=β0+β1x1+β2x2+β1,2x1∗x2
When we include the vaccine uptake x population density interaction term, yes, it influences the model.
New Cases=−2916.185+65.0054⋅Vax Uptake+39.4434⋅PopDen−0.4707⋅Vax Uptake∗PopDenNew Cases=−2916.185+65.0054⋅Vax Uptake+39.4434⋅PopDen−0.4707⋅Vax Uptake∗PopDen
In this model, PopDen and VaxUptake*PopDen and the overall model are all significant (p<0.05). (Here “*” means “times”, as in “multiplied by”.)
Unfortunately, the m1 slope parameter is even more positive (65.0054) under the full model. And that is a big deal because even the full model is significant (p<0.05).
Model 1 full results. Model 2 full results.
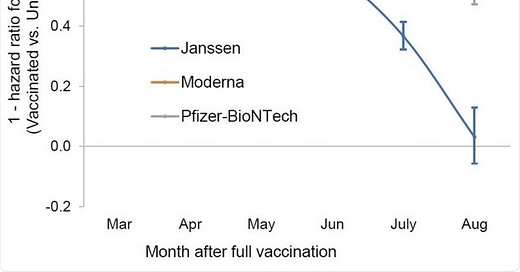
Combined with the positive slope in the country-level analysis, the Israeli data, the UK data, and the data from Barnstable County, Massachusetts, the data from Gibraltar (140% vaccinated and they canceled Christmas), and my prior country-level analysis, these data suggest that the hypothesis that the vaccine is contributing to the spread of the SARS-CoV-2 virus seems to be a viable concern.
This is not entirely unexpected given the fact that vaccination lead to consistent pathophysiological alterations seen in this study in Nature (Liu et al., 20201), which reported that after vaccination, patients showed:
“Reduction of CD8+ T cells and increase in classic monocyte contents were exemplary. Moreover, scRNA-seq revealed increased NF-κB signaling and reduced type I interferon responses, which were confirmed by biological assays and also had been reported to occur after SARS-CoV-2 infection with aggravating symptoms. Altogether, our study recommends additional caution when vaccinating people with pre-existing clinical conditions, including diabetes, electrolyte imbalances, renal dysfunction, and coagulation disorders.”
Low CD8+ T cells are a signature of long-haul COVID-19. Dr. Bruce Patterson told me this in our Jan 31, 2020 interview on Unbreaking Science.
Further, the recent Wang et al. (2021) included the observation that vaccination of individuals using antigens from extinct variants of SARS-CoV-2 may disrupt the ability of our antibodies to effectively deal with new SARS-CoV-2 variants* means a few things. One fact is that the current vaccines cannot be expected to do anything other than make the situation worse. Perhaps this was always so, depending on the rate of evolution of vaccine escape, and the degree of variability of spike protein that emerges in infected individuals as result of immune pressure.
The second important points is people with healthy immune systems may fare both vaccination and infection better, but that in countries where the primary immunologic target has been the spike protein via spike-only vaccination, individuals who are vaccinated may be at higher risk of disease enhancement due to the exclusivity of their narrow immunity, compared to individuals who have survived SARS-CoV-2 infection due to multi-epitope immunity. Ask your doctor if the Brownstein protocol maintenance protocol is right for you.
The prediction is that in the first two weeks of vaccination uptake, individuals may be made more susceptible to SARS-CoV-2 infection (and other infections) due to the immune suppressive effects of SARS-CoV-2 viral proteins.
Combine that with the fact that “breakthrough infections” - infections in the vaccinated - have as high viremia as the unvaccinated, and anyone can see we have a significant problem. (Source)
By comparison, here’s Fauci’s level of understanding of all of this, just a couple of weeks ago:
“If you're vaccinated — and hopefully you'll be boosted too — and your family is, you can enjoy a typical Thanksgiving meal.” (Boston. com)
This is inconsistent with the guidance from CDC Director Rochelle Walensky, who, upon seeing the Barnstable County, Massachusetts data, said that the vaccinated are still at risk of contributing to the spread of COVID-19 and should socially distance and mask TO PROTECT OTHERS. (Source.)
Most disturbing of all, Fauci said this knowing that the vaccinated can spread COVID-19, just like he knows the vaccinated can spread Mumps and Pertussis.
If you’re vaccinated, and you think you are not likely to spread COVID-19, think again.
*NOTE: THE MUTATIONS IN THE MRNA LEAD TO AMINO ACID CHANGES THAT CHANGE THE SHAPE OR CHARGE OF THE EPITOPE ENOUGH TO CAUSE ANTIBODIES FROM PRIOR EXPOSURE TO THE ORIGINAL ANTIGEN TO NO LONGER BE ABLE TO BIND AND NEUTRALIZE THE VIRUS CARRYING THE CHANGED EPITOPES. THIS IS ALSO KNOWN AS ORIGINAL ANTIGENIC SIN. See this letter published by Cambridge University on Original Antigenic Sin, it explains it quite well.
References
Liu et al., 20201. Comprehensive investigations revealed consistent pathophysiological alterations after vaccination with COVID-19 vaccines https://www.nature.com/articles/s41421-021-00329-3
Study: Fully vaccinated people with "breakthrough" COVID Delta infections carry as much virus as the unvaccinated. https://www.cbsnews.com/news/covid-vaccine-delta-variant-infections-carry-same-virus-load-unvaccinated/
Patterson, B. 2021. Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning. https://www.frontiersin.org/articles/10.3389/fimmu.2021.700782/full
Pouwels KB, Pritchard E, Matthews PC, Stoesser N, Eyre DW, Vihta KD, House T, Hay J, Bell JI, Newton JN, Farrar J, Crook D, Cook D, Rourke E, Studley R, Peto TEA, Diamond I, Walker AS. Effect of Delta variant on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. Nat Med. 2021 Oct 14. doi: 10.1038/s41591-021-01548-7. Epub ahead of print. PMID: 34650248. https://www.nature.com/articles/s41591-021-01548-7.pdf
Wang et al., 2021. Mechanisms of SARS-CoV-2 Evolution Revealing Vaccine-Resistant Mutations in Europe and America. J Phys Chem Lett 12:11850-11857 https://pubs.acs.org/doi/full/10.1021/acs.jpclett.1c03380
Find the peer-reviewed Brownstein protocol here.
Related:










Excellent work! I couldn't agree more.
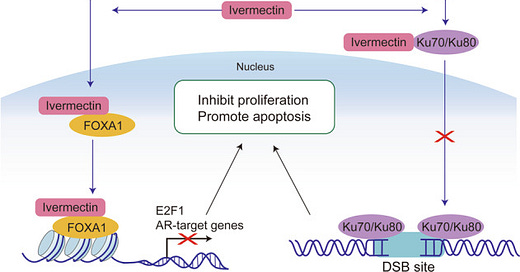
Get a load of this. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8538446/
Severe acute respiratory syndrome coronavirus 2 (SARS–CoV–2) has led to the coronavirus disease 2019 (COVID–19) pandemic, severely affecting public health and the global economy. Adaptive immunity plays a crucial role in fighting against SARS–CoV–2 infection and directly influences the clinical outcomes of patients. Clinical studies have indicated that patients with severe COVID–19 exhibit delayed and weak adaptive immune responses; however, the mechanism by which SARS–CoV–2 impedes adaptive immunity remains unclear. Here, by using an in vitro cell line, we report that the SARS–CoV–2 spike protein significantly inhibits DNA damage repair, which is required for effective V(D)J recombination in adaptive immunity. Mechanistically, we found that the spike protein localizes in the nucleus and inhibits DNA damage repair by impeding key DNA repair protein BRCA1 and 53BP1 recruitment to the damage site. Our findings reveal a potential molecular mechanism by which the spike protein might impede adaptive immunity and underscore the potential side effects of full-length spike-based vaccines.