Stanford University Research: New Autoimmune Regulator Found in Humans: KIR+ T-Cells
In mice, KIR+ T cells have been shown to regulate rogue T cells that cause autoimmune disease. Now we know about KIR+ T cells in humans and how important they are to immune tolerance in humans
Good morning, Popular Rationalists. Put your brain on, this is important and very cool.
T-cell malfunction can cause autoimmunity. Often, rogue T-cells initiate an intense inflammatory response against our own proteins.
At Stanford University, two scientists - Jing Li and Maxim Zaslavsky - wanted to know whether KIR+ T-cells, which were known to regulate the rogue autoreactogenic T cells in mice, could be found in action regulating autoimmune disease in humans by regulating a type of cell called a CD4 cell.
They chose patients with celiac disease. Their studies examined patients with celiac diseases who ate gluten vs. those who ate gluten-free diets. The scientists wanted to know if KIR+ T cells were more abundant in the guts of patients with celiac disease exposed to gluten.
Their results? There were more KIR+ T cells in the patients who ate gluten. The KIR+T cells also directly killed rogue celiac disease-causing T cells as their mechanism of action in regulating the autoimmune response.
Looking further at different autoimmune diseases, including celiac disease, multiple sclerosis, and systemic lupus erythematosus. The scientists want to know if perhaps the KIR+ T cell regulation of CD4+ T cells is a general mechanism that helps our bodies undergo normal immunological tolerance, stopping self-reactive T cells from causing harm.
Popular Rationalist readers will anticipate, given their understanding of pathogenic priming and its role in severe COVID-19, whether KIR+ T cells appear to be involved in preventing severe COVID-19.
Zaslavsky and Li did indeed find these KIR+ T cells in patients with COVID-19, and that patients with more severe COVID-19 symptoms had a stronger KIR+ T cell response than patients with mild disease. It seems likely that this could at least indicate that the immune tolerance mechanism is being challenged by the actions of the rogue T cells in these severe COVID-19.
This is exciting research because (among other things) it is possible that people might be able to bring flares of autoimmune disease under control. Flares can be painful, disabling, and life-threatening.
Further, if there is a genetic basis for aberrant CD4 cell activity during infection, the risk of both pathogen-induced autoimmunity and vaccine-induced autoimmunity might be better understood.
Note to reader: I’m so glad you are part of the Popular Rationalist community! Cheers.
Citation: Li, J, and Zaslavsky, M, et al. KIR+CD8+ T cells suppress pathogenic T cells and are active in autoimmune diseases and COVID-19. Science 376, eabi9591 (2022
It’s not too late to enroll in The Biology of Immunology at IPAK-EDU and learn the fundamentals of our immune systems! We go deep!
PRICE DROPPED TO $80! 50% off! (Classes are live - you can view past lectures or any you miss after the class).
Check it out!
Study Abstract: Previous reports show that Ly49+CD8+ T cells can suppress autoimmunity in mouse models of autoimmune diseases. Here we find a markedly increased frequency of CD8+ T cells expressing inhibitory Killer cell Immunoglobulin-like Receptors (KIR), the human equivalent of the Ly49 family, in the blood and inflamed tissues of various autoimmune diseases. Moreover, KIR+CD8+ T cells can efficiently eliminate pathogenic gliadin-specific CD4+ 10 T cells from Celiac disease (CeD) patients’ leukocytes in vitro. Furthermore, we observe elevated levels of KIR+CD8+ T cells, but not CD4+ regulatory T cells, in COVID-19 and influenza-infected patients, and this correlates with disease severity and vasculitis in COVID-19. Expanded KIR+CD8+ T cells from these different diseases display shared phenotypes and similar T cell receptor sequences. These results characterize a regulatory CD8+ 15 T cell subset in humans, broadly active in both autoimmune and infectious diseases, which we hypothesize functions to control self-reactive or otherwise pathogenic T cells.
One-Sentence Summary Here we identified KIR+CD8+ T cells as a regulatory CD8+ T cell subset in humans that suppresses self-reactive or otherwise pathogenic CD4+ 20 T cells.




One of the reasons I never took the clot shot is that I’m aware that everything about the workings of the immune system is NOT fully understood. Medical science is figuring out new aspects every day...so don’t gamble with some novel technology!
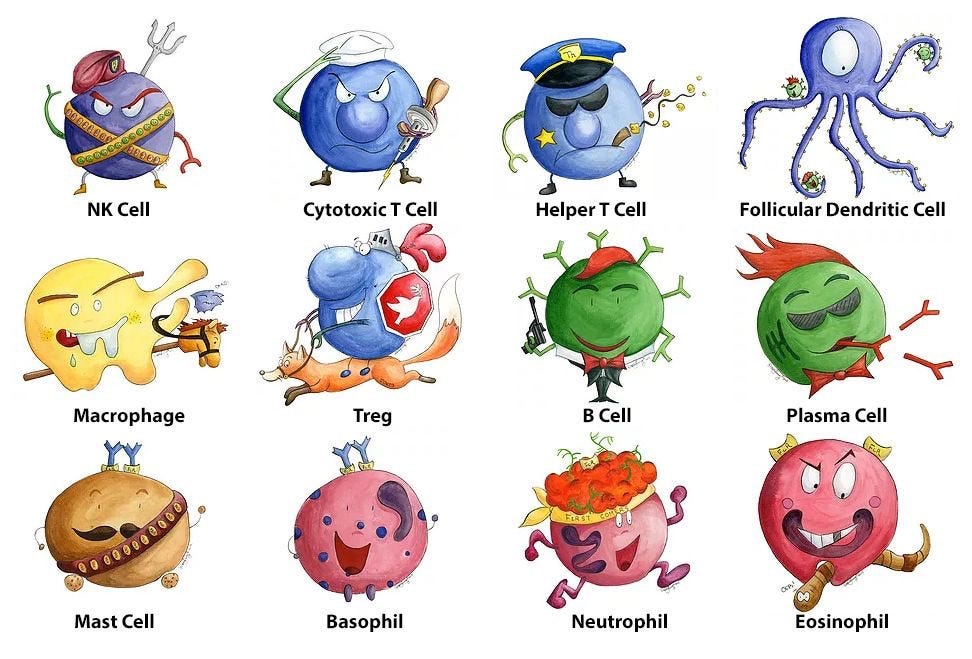
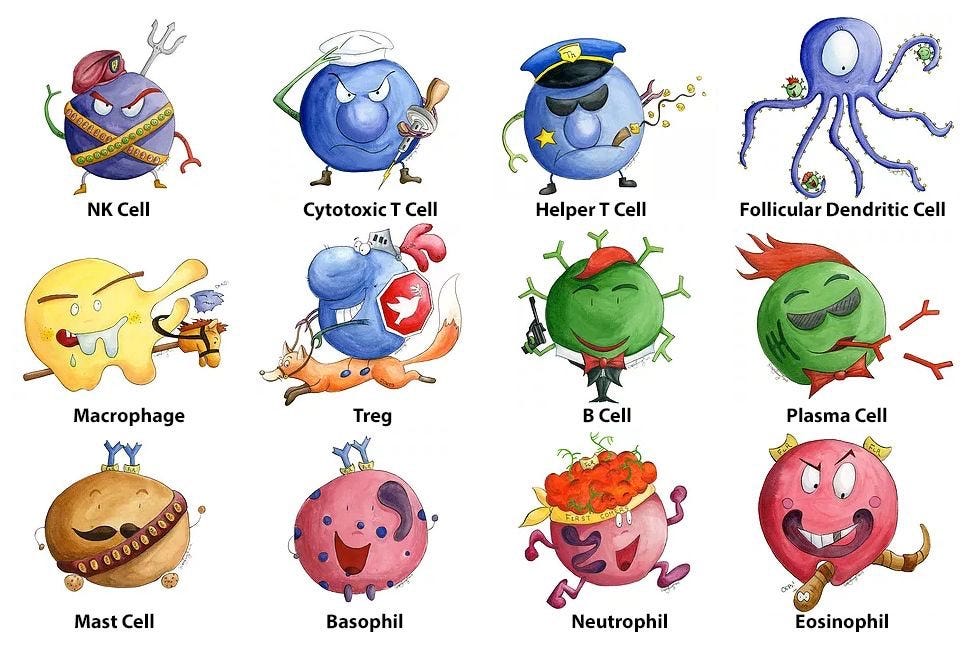
Love the comic representations of cells.