Myocarditis Risk from the Vaccine vs. Virus: the UK Study
One study says the risk is higher than baseline. Another says the risk is higher from the virus. Let's dive in and look at these studies in-depth.
We’ve seen dozens of strong, vibrant vaccinated athletes dropping like flies in Europe (we'll I’ve seen it, the MSM in the US has been recklessly silent on that issue). We do not yet know if these athletes are dropping due to a second exposure via infection following vaccination, or to the effects of vaccines alone.
(NB: UK Guidance paragraph removed due to differences in durations of periods)
There are two new studies on myo/pericarditis; one from Ontario that confirms higher risk of myocarditis following vaccination compared to baseline, and another study that alleges to show higher risk of myocarditis following infection compare to vaccination (Nature journal).
I want to point also to this Reuters article’s headline “Higher risk of heart complications from COVID-19 than vaccines -study” and the article, which leaves out a critical detail about the Nature UK study, which does not actually support the article’s conclusion. And the Ontario study it appears is being misinterpreted.
First, let’s compare the two studies and find how the two studies are, or are not comparable and see what, if anything, we can clear up.
Study 1. “Epidemiology of myocarditis and pericarditis following mRNA vaccines in Ontario, Canada: by vaccine product, schedule and interval” (medrxiv.org)
Population: Ontario, Canada (14.7 million) who received at least one dose of COVID-19 mRNA vaccine between December 14, 2020 and September 4, 2021.
Data source: Provincial COVID-19 vaccine registry and Provincial adverse events following immunization database
Exposure: Pfizer or Moderna
Doses: 19,740,741
Period: Any time
Cases: N/A
Myocarditis/pericarditis events: 297
Notes: Rates higher with shorter interval between vaccines, or when mixing mRNA vaccines.
Study type: Population-based cohort study using passive vaccine safety surveillance data
Overall rate, vaccinated: 1.5 per 100,000 doses
Overall rate, infected: xx per infection (not studied)
Overall rate, vaccinated, per population size: 2.98 per 100,000 people
Result:
There were 0.625 events per 100K with one dose (all ages).
There were 3.35 events per 100K with two doses (all ages).
From their data, I estimate that myo/pericarditis is occuring at 62-78 times the expected rate in young males in the “fully vaccinated” with two doses.
Author’s Conclusion: “Our results suggest that vaccine product, inter-dose interval and vaccine schedule combinations may play a role in the risk of myocarditis/pericarditis, in addition to age and sex. Certain programmatic strategies could reduce the risk of myocarditis/pericarditis following mRNA vaccines.”
Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination is higher than from SARS-CoV-2 infection
Study 2. “Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection”
Study type: Self controlled case series (SCCS)
Population: England <40 years of age (approx. 34,649,214) receiving at least one dose of vaccine between December 1, 2020 and August 24, 2021
Data source: The English National Immunisation (NIMS) Database of COVID-19 vaccination
Exposure: ChAdOx1, BNT162b2 or mRNA-1273 vaccines
Doses: 38,615,491
Period: 1-28 days following vaccination (vaccinated), -28 to -1 days prior to vaccination (unvaccinated, infected)
COVID-19 Cases (pre-vaccination): 61 (From Table 3)
Myocarditis/pericarditis events following vaccination: 746 (From Table 3)
Note: Ascertainment bias due to SARS-CoV-2 admission screening. SCCS study design is susceptible to temporal confounding (changes in conditions over time). The authors acknowledged these limitations, which can be substantial.
(Dear Reader: As always, feel free to check my math and comment if you disagree with these).
Overall myo/pericarditis rate, vaccinated (any time) =1,615/38,615,491*100,000 = 4.18 /100K vaccinated persons
Overall myo/pericarditis rate, vaccinated, 1-28 days: 1.931 per 100,000 doses
Overall myo/pericarditis rate, per population size, 1-28 days: 2.153 per 100,000 persons
Notes: The authors chose the result from the analysis in which myo/pericarditis data in the not-yet-vaccinated were limited to 1-28 days preceding receipt of the vaccine, and myo/pericarditis data in the vaccinated were limited to the 1-28 days following the vaccine.
Author’s conclusion: “First, there was an increase in the risk of myocarditis within a week of receiving the first dose of both adenovirus and mRNA vaccines, and a higher increased risk after the second dose of both mRNA vaccines. In contrast, we found no evidence of an increase in the risk of pericarditis or cardiac arrhythmias following vaccination, except in the 1–28 days following a second dose of the mRNA-1273 vaccine. Second, in the same population, there was a greater risk of myocarditis, pericarditis and cardiac arrhythmia following SARS-CoV-2 infection. Third, the increased risk of myocarditis after vaccination was higher in persons aged under 40 years.”
There are a number of reasons to draw into question the main conclusion of this study, which was that the risk of myocarditis/pericarditis following infection with SARS-CoV-2 virus is higher than the risk following vaccination.
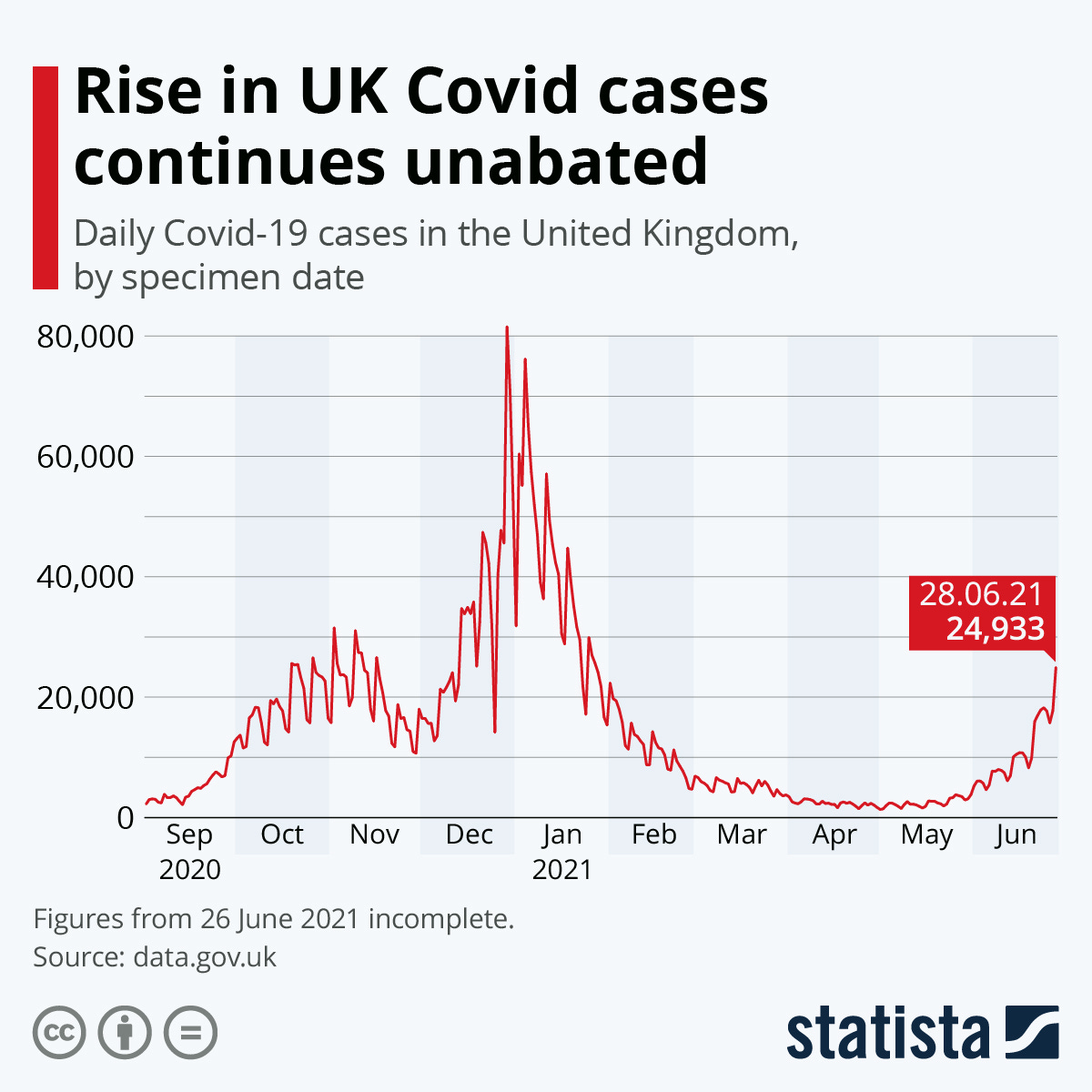
First, the IRR in this study was relative to events in the baseline period (Dec 2020 - Aug 2021). During this time, the number of cases shifted; it peaked in January 2021 and then steadily declined overall until the more recent post-vaccination effort surge. The SCCS study design is sensitive to temporal confounding; with the rates higher or lower in the near past, the comparison of rates comparing recent individuals to self in the past can be hazardous.
The authors knew this, and thus they reported that “(a) prerisk interval of 1–28 days before each exposure date was included to account for potential bias that might arise if the occurrence of the outcome temporarily influenced the likelihood of exposure.” They also “adjusted for week” to accommodate variation associated with seasonality.
However, the likelihood of exposure should not influence the probability of adverse event, so the logic of preferring the result from the restricted analysis of events 1-28 days before vaccination is not justified.
Nevertheless, the authors reported during the baseline period there were 119 events per 216.7 person-years. That is 119/216.7 or 0.549 events/pyrs. Their Table 3 is large and can be confusing, but I spent a lot of time decoding it, and found some strange facts:
The day-of-vaccination results are “suppressed”, without any explanation or justification other than small sample size for the Moderna vaccine not offered at the youngest age group.
The denominator “person years” is not defined anywhere in the text or Supplementary material.
The “person years” number is the same, or nearly the same, for each weekly period of vaccine-related events, but varies for the infection-related events. This seems unlikely as people die over time from other causes. The authors therefore have derived a “sketchy denominator”. (NB: Vaccination risk is clustered in a short period of time because many people are vaccinated rapidly; infection risk is spread out over a longer period of time because the rate of transmission is slower than the vaccination program.)
The details of the PCR testing are not clear; for example, it is not clear if people who are vaccinated are diagnosed in the same manner as those who are not vaccinated (same Ct threshold cut-off). The diagnostic results are also not verified by sequencing.
The 1-28 period length in both directions is arbitrary; why not study baseline rates over the entire time period, and increase the power of the test with larger total numbers both in the numerator and in the denominator? We have an ongoing, live proposed whole-population experiment, with two time periods: the onset of COVID-19 (January, 2020) to present, and the start of vaccination (varying dates per vaccine) to present. Why then the arbitrary 28-day cut-off? Why any cutoff?
The period of time is a very important factor in both studies. There are no data supporting a 28-day cutoff in either direction for the UK study; this is an utterly arbitrary design aspect seen in other vaccine safety studies that ultimately becomes false justification for policy and law decisions (such as cases in the NVICP). In research studies, the time cut-offs for considering events are assumed; in vaccine court, the same arbitrary cut-offs for considering events become enforced, leading to circular reasoning.
A straightforward and fair comparison would be “the number of events in unvaccinated persons since January, 2020” vs “the number of events in vaccinated persons per one- or two-dose exposure” per day. If there is concern over temporal shifts in the rate of myo/pericarditis in the unvaccinated and in the vaccinated, this should be justified using data or temporal trends in myo/pericarditis, not using shifts in infection. The data could be easily matched temporally from the start of each vaccine type.
Another issue is one of representativeness. Every person in the UK study was vaccinated. This can lead to selection bias; individuals who tend to not vaccinate might include those who already had COVID-19. The non-vaccinating population will also be relatively free from aluminum (a vaccine adjuvant), less likely to have received all other vaccines and thus less susceptible to autoimmunity due to the vaccine adjuvants, and less likely to suffer impaired immune response due to exposure to ethylmercury in thimerosal, which inhibits the protein ERAP1. They may also not vaccinate because they have familial or person history of vaccine injury, or autoimmunity. Ultimately, the study sample may not be representative of the entire population. The bias could go in the other direction as well; people with past episodes of myo/pericarditis might eschew the vaccination program out of fear of a repeat onset.
Disease Burden from Dual Exposures Not Considered
Disease burden is not restricted to a 28-day period for the virus, and it should not be restricted for the vaccine. Given the low prevalence of viral infection, and the high incidence of vaccination, the total number of cases, hospitalizations and deaths attributed to vaccination and the number attributed to the virus is more relevant than rates.
This is complicated, however, because the vaccinated are double-exposed; they may have had prior or subsequent infection. This certainly leads to misattribution, and could amplify or dampen their responses “to the vaccine”. Thus, clearly, “exposure to the vaccine-only” is not a clinical option for the vaccinated. The comparisons in the UK study are off-target. The vaccinated who get a SARS-CoV-2 infection may be primed by the vaccine to experience clinical effects of their likely future (some say inevitable) infection, and vice versa. People who are infected first, of course, likely do not mount a spike-only immune responses, so the risk of pathogenic priming will likely be muted in any one individual, but spread out over a larger population as genetic variation causing homology between human and viral proteins will tend to reach more people.
The UK study reports that length of hospital stay was shorter for those who developed myocarditis within the 28-day window following vaccination compared to cases “whose admissions had not occurred in the 28 days post vaccination”. Note this would include persons admitted on days 29+ following vaccination.
With all of these moving parts, the last thing we need is complex studies that do not address straightforward, relevant questions.
The focus should be on the cardiac-related disease burden attributable to the vaccination, and that attributable to the infection, so the correct comparison would be “cardiac events in the immune from infection” relative to “cardiac events in the vaccinated who have not been infected, even though they are not likely immune” relative to the exposed population size - and the vaccinated population should have been tested for signs of prior- and post-vaccination infection.
The UK Study is Entirely Problematic
The authors of such studies appear unaware of the risk of disease enhancement and the horrific effects of mass vaccination on priming huge numbers of people for more serious illness of myriad type following their eventual infection by a SARS-CoV-2 variant (disease enhancement). All of the events in the pre-vaccinated period are attributed to infection, and none of the events in the post-vaccinated period are attributed to infection, as if the vaccines prevent infection. They do not. The clinical and public health community is well aware of disease enhancement and pathogenic priming; dual exposure is unaccommodated in this study.
The time-frame for pathogenic priming is not 28 days. The UK study especially uses inexact thinking, for example, correcting for temporality in COVID-19 rates, not equalizing for established temporal variation myocarditis, and studies populations that do not accurately represent the clinical populations involved.
Hospitalization trends show that all vaccinated persons will likely be exposed to the SARS-CoV-2 virus. Some of the infected vaccinees will transmit, some will be hospitalized, and some will die. It is entirely clear that SARS-CoV-2 will circulate regardless of vaccination coverage given the vaccines at hand. Thus, the clinical groups of interest should be redefined to insure representativeness, and the data re-analyzed reflecting the clinical realities of surging COVID-19 in a mostly vaccinated country.
I encourage you to read Jeremy Hammond’s very recent article on the AAP’s misrepresentation of the result on myocarditis risk in children from COVID-19. In that article, he’s addressing a different study (by CDC), but finds similar issues:
“For the president of the AAP to equate the myocarditis risk among hospitalized children with the risk for all children who are infected is not only unscientific but willfully dishonest.
The CDC’s study design introduces ascertainment bias, which in this case is a selection bias that is likely to result in an overestimation of the overall risk of myocarditis in children with SARS-CoV-2 infection. For our purposes, we can safely assume that the CDC’s estimate of the risk of myocarditis among patients with COVID-19 is an upper bound in terms of generalizability to all children who are infected.”
It’s a good read, and I admire Jeremy’s acumen.
Related:
Hammond, J. 2021. AAP Lies about Myocarditis Risk to Children from COVID-19 Vaccine https://www.jeremyrhammond.com/2021/12/16/aap-lies-about-myocarditis-risk-to-children-from-covid-19-vaccine/
Here, Vinay Prasad seems to think the Ontario study shows higher risk of myocarditis in the vaccinated than in the unvaccinated. He must mean higher than baseline, which I believe he took to reflect “unvaccinated”. However, the baseline was pre-COVID-19. Check me on that, and leave a comment if you agree or disagree.



Please see the Billy Eduard Albert Meier (BEAM) Contact Report 787 warning on the vaccinations (https://www.futureofmankind.info/Billy_Meier/Contact_Report_787):
"The fact that, according to our observations, around ⅘ of the dead from the Corona epidemic for some time now are not unvaccinated persons, but persons who have been vaccinated once or several times with the inadequate vaccines, is mendaciously presented to the contrary."
"The fact remains, however, that those who have been vaccinated can spread the Corona epidemic and thus infect the unvaccinated and those who have already been vaccinated, just as they can infect the so-called ‘cured’ with the epidemic pathogen again. The so-called experts know this very well, but they keep quiet about it and suppress the truth from the public, because the public is of the opinion that immunity is caused by the development of antibodies through vaccination."
Early in this post you write: "A Guidance from the UK is clear: Moderna has 36 events per 100,000 doses; that’s twice per person compared to 36 events per 100K in the baseline data."
The sentence is confusing in its own right, and the mystery deepens when one clicks on your link to the UKHSA guidance. That guidance states that as of mid-November, there were 36 cases of myocarditis reported per 1,000,000 (not 100,000!) doses of the Modern vaccine. And it states that in study of a roughly 20 year period of NHS hospital admissions, myocarditis represented approximately 36 per 100,000 admissions. These statistics are not straightforwardly comparable, and your decimal error aside, it's not clear what comparison you intended to draw (or note) between them.