Viruses and Accelerated Aging Provide Key Insights on Expected Effects of Repeated Exposures to SARS-CoV-2 Spike Proteins
No one wants premature aging. But science says that what’s in store for the hypervaccinated.
BASIC UNDERSTANDING OF THE PATHOPHYSIOLOGY OF THE SPIKE PROTEIN INFORMS US THAT THE VACCINATED SHOULD AGE FASTER AND HAVE MORE CHRONIC ILLNESS, AS SHOULD THEIR IMMUNE SYSTEMS. THIS IS A COMPLETE REFERENCE RESOURCE FOR YOURSELF, YOUR DOCTORS AND YOUR LAWYERS.
The last decade of research in immunology has led to advances in understanding how viruses can lead to accelerated aging. The relationship between persistent viral infections and accelerated aging in particular garnered significant attention in the scientific community. Considering first mechanisms by which viruses can hasten the aging process, we will then contemplate the effects of repeated exposures to SARS-CoV-2 spike proteins.
The Aging Burden of Persistent Viral Infections
Persistent viral infections, particularly those caused by herpesviruses, have been shown to exacerbate the decline of the immune system, a phenomenon termed immunosenescence. This study published in AGING RESEARCH REVIEWS highlights how these infections drive T cells into a state of exhaustion. This chronic immune activation not only strains the immune system but also accelerates its aging.
The van den Bossche effect is a different matter; his concern is evolutionary IMMUNE ESCAPE. Immune escape refers to the ability of a virus to mutate and evolve in a manner that allows it to evade the immune response. This can happen through changes in the virus's surface proteins, which are the primary targets of the immune system's antibodies. (See, for example In Anticipation of a Highly Virulent SARS-CoV-2 Variant (substack.com)).
Others expect only the survival and transmission of less lethal variants due to the loss of lethal variants from high morbidity and mortality given the trade-off between transmissibility and and mortality. In viral evolution, the trade-off between transmissibility and mortality (commonly referred to as the "virulence-transmission trade-off" or simply the "trade-off hypothesis") posits that over time there is a balance between a virus's ability to spread (transmissibility) and the severity of the disease it causes (virulence or mortality).
The trade-off hypothesis works because if a virus is too virulent and kills its hosts rapidly, it may reduce its chances of transmission, as severely ill or deceased hosts are less likely to interact with others and spread the infection. Conversely, if a virus is highly transmissible but causes less severe disease, it can spread more effectively through the population. Over time, this evolutionary pressure can lead to the emergence of strains that are more contagious but potentially less deadly, as they can sustain their transmission by not incapacitating their hosts too severely.
In a system as complex as human society, some of whom are attempting to acquire personal immunity via vaccination and others not, the adaptive immunological landscape for the virus will have two peaks - if the vaccine has positive efficacy. Once the vaccine achieves negative efficacy, fewer people will continue to accept “booster”, and the landscape will shrink toward primarily natural immunity.
Inflammaging - Aging and Immune System Decline
As we age, our immune system gradually deteriorates. This well-characterized decline is multifaceted, involving thymus involution, cellular senescence, and chronic low-grade inflammation, known as inflammaging. A comprehensive review in Lancet Infectious Disease discusses how aging may be both a cause and a consequence of infection, with enhanced inflammation and pathogen-dependent mechanisms playing pivotal roles, one feeding back on the other.
This source of inflammation will confuse some clinicians as either “a normal part of aging” or misdirect them, for some patients toward autoimmunity (e.g., via increased C-reactive protein, or even antinuclear antibodies) toward occult disease like autoimmunity when, in fact, the repeated exposures may lead to increased inflammation with or without pathogenic priming.
The Vicious Cycle of Infections and Aging
The intersection of aging and infections creates a vicious cycle. Older adults are more susceptible to infections due to a weakened immune system. In turn, these infections can further impair immune function. For instance, Frontiers in Medicine reports that infections are leading causes of morbidity and mortality in the elderly, with factors like immunosenescence and comorbid chronic diseases contributing to this increased vulnerability.
The Role of Immunosenescence
Immunosenescence both increases susceptibility to infections and diminishes the body's ability to respond to vaccinations, as discussed in an article from Frontiers in Immunology. This reduced response is particularly evident in the context of respiratory infections like influenza and pneumonia, which are more common and severe in older adults.
Implications for COVID-19 Vaccination
The relationship between persistent viral infections and accelerated aging is a testament to the complexity of the human immune system. Understanding this relationship is crucial for developing strategies to mitigate the effects of aging and improve the health outcomes of the elderly population. As research in this field continues to evolve, it offers promising insights into enhancing longevity and quality of life in our later years.
But it also informs us that we should not expose anyone repeatedly and chronically to the SARS-CoV-2 spike protein.
Over the last two years, significant progress has been made in understanding the pathophysiological mechanisms of the SARS-CoV-2 spike protein. Here are some key findings:
1. Virus Entry and ACE2 Receptor Binding
The SARS-CoV-2 spike protein facilitates the virus's entry into cells by binding to the angiotensin-converting enzyme 2 (ACE2) receptor. This interaction is a critical step in the virus's life cycle and pathogenesis. Nature and Physiology provide detailed insights into this mechanism.
2. Spike Protein Structure and Function
The spike protein is a trimeric glycoprotein that undergoes significant conformational changes to mediate fusion between the viral and host cell membranes. This process is essential for the virus's entry into host cells. Nature Reviews Microbiology discusses the structure and function of the spike protein in detail.
In its fusion to the host cell membrane, spike is known to cause syncytia - combined cells caused by the gluing together of membranes. In its expression on the surface of the host cell, spike causes similar havoc.
Here are some key studies and articles providing evidence and discussion on the SARS-CoV-2 spike protein causing syncytia formation:
Syncytia Formation during SARS-CoV-2 Lung Infection
Citation: Buchrieser, J., Dufloo, J., Hubert, M., Monel, B., Planas, D., Rajah, M. M., ... & Schwartz, O. (2021). Syncytia formation during SARS-CoV-2 lung infection. Cell Death & Differentiation, 28(9), 2765-2777. [Link]
Summary: This study discusses how the SARS-CoV-2 spike protein can induce syncytia formation, especially when specific sequences are inserted at the S1/S2 cleavage site.
The Mechanism and Consequences of SARS-CoV-2 Spike Protein-Induced Syncytia
Citation: Braga, L., Ali, H., Secco, I., Chiavacci, E., Neves, G., Goldhill, D., ... & Noursadeghi, M. (2021). The mechanism and consequences of SARS-CoV-2 spike protein-induced syncytia. Journal of Infection, 83(3), 237-279. [Link]
Summary: This article explains how SARS-CoV-2 induces syncytia when the viral spike protein on the surface of an infected cell interacts with receptors on neighboring cells.
SARS-CoV-2 Spike Protein Dictates Syncytium-Mediated Lymphocyte Elimination
Citation: Cattin-Ortolá, J., Welch, L. G., Maslen, S. L., Papa, G., James, L. C., & Munro, S. (2021). SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination. Cell Death & Differentiation, 28(9), 2765-2777. [Link]
Summary: This study focuses on how the SARS-CoV-2 spike protein can lead to syncytium formation, which in turn may contribute to lymphocytopenia observed in COVID-19 patients.
Cell Fusion as a Link between the SARS-CoV-2 Spike Protein, COVID-19 Pathology, and Syncytia
Citation: Sattentau, Q. J., & Moore, J. P. (2021). Cell fusion as a link between the SARS-CoV-2 spike protein, COVID-19 pathology, and syncytia. Journal of Experimental Medicine, 218(12), e20211381. [Link]
Summary: This article discusses the distinctive feature of the SARS-CoV-2 spike protein in efficiently fusing cells, thus producing syncytia found in COVID-19 patients.
There are others, including syncytia formation among cardiac cells, brain cells, and others.
Recent research has shed light on the effects of the SARS-CoV-2 spike protein on cardiac cells. Here are some key findings from recent studies:
SARS-CoV-2 Spike Protein and Cardiovascular Disease
Citation: Lei, Y., Zhang, J., Schiavon, C. R., He, M., Chen, L., Shen, H., ... & Chen, Z. (2022). SARS-CoV-2 spike protein impairs endothelial function via downregulation of ACE 2. Circulation Research, 128(9), 1323-1326. [Link]
Summary: This study demonstrates that the SARS-CoV-2 spike protein can increase cardiac pericyte migration and reduce endothelial cell network formation, contributing to cardiovascular disease.
Coronavirus Spike Protein and Heart Muscle Damage
Citation: [AHA Newsroom]
Summary: Research indicates that the spike protein from SARS-CoV-2 causes heart muscle damage, emphasizing the importance of vaccination to prevent such effects.
Spike Protein and Heart Vascular Cell Damage
Citation: [Nature Community]
Summary: This article discusses the strategy adopted by SARS-CoV-2 to damage heart vascular cells, highlighting the role of the spike protein in this process.
Spike Protein Leading to Heart Muscle Injury
Citation: [Medical News Today]
Summary: Experiments suggest that the SARS-CoV-2 spike protein can lead to heart muscle injury, potentially through an inflammatory process.
Inflammatory Effects of the Spike Protein on the Heart
Citation: [News-Medical.Net]
Summary: The spike protein is not only directly damaging to heart muscle cells but also highly inflammatory, potentially causing systemic inflammation that affects the heart.
These studies provide insights into how the SARS-CoV-2 spike protein can affect cardiac cells, highlighting its role in causing direct damage to heart muscle cells and contributing to cardiovascular complications associated with COVID-19.
Since SARS-CoV-2 spike protein causes syncytia formation, a process that contributes further to the pathophysiology of exposure to spike, repeated exposures to spike can only accelerate cell death, tissue and organ inflammation, and the resulting -opathies seen following vaccination and/or infection.
Immune Response Evasion
SARS-CoV-2 has evolved mechanisms to evade the host immune response, partly mediated by its spike protein. The spike protein can undergo mutations that enhance its binding affinity to ACE2 or allow it to escape neutralizing antibodies. PNAS provides information on how the spike protein contributes to immune evasion.
This was among Dr. van den Bosshe’s original concerns. Adding in T-cell exhaustion, we can fully expect immunosenescence and thus increased susceptibility to viruses other than SARS-CoV-2 among the vaccinated.
Induction of Hyperinflammation
The interaction of the spike protein with the ACE2 receptor can also trigger a hyperinflammatory response, leading to severe disease manifestations like acute respiratory distress syndrome (ARDS). This aspect is covered in studies available review in TRENDS IN IMMUNOLOGY. This mechanism of pathophysiology is not restricted to the virus.
Impact on Vascular and Organ Systems
Beyond the respiratory system, the spike protein has been implicated in affecting other organ systems, including the cardiovascular system, contributing to conditions like myocarditis and thrombosis.
I won’t include my #PATHOGENICPRIMING as that has been the subject of so much ongoing research that it is easily accessible in other articles here and widely cited elsewhere. (CITED BY IN PUBMED (63); CITED BY IN GOOGLE SCHOLAR, 205).
SUMMING UP
From this understanding of these pathophysiologic effects of the spike protein, chronic exposure to the spike protein, particularly through repeated infections, should by now be understood to exacerbate the immune system's response, leading to a state of chronic inflammation, immune system overactivation, and immune exhaustion. This should increase the risk of developing conditions associated with hyperinflammatory states, such as cardiovascular complications or autoimmune disorders, and it should leave the hypervaccinated at increased risk of all manner of infections. All of this occurs in addition to pathogenic priming and antibody-dependent enhancement.
Additionally, we can expect that continuous and repeated exposure should contribute to the acceleration of immunosenescence, the gradual deterioration of the immune system associated with aging.
So repeated exposure to the spike protein should be expected by now to result in a reduced ability to fight off not only SARS-CoV-2 but also other pathogens - just on its mechanisms of disease-making. Furthermore, the spike protein's potential impacts on other organ systems, as indicated by studies showing its effects beyond the respiratory system, suggest that chronic exposure should be expected to have wide-ranging negative implications for long-term health.
SOLUTIONS
If you received a COVID-19 jab, I highly recommend first asking the doctor who vaccinated you for solutions to these problems. Print out this article share it with them, and ask them for their opinion. When they bluster, misdirect, and lie to you about your symptoms not being caused by the COVID-19 vaccines, you can then educate them about the doctors doing the hard work of identifying protocols that minimize, but sadly so far do not reverse, the chronic health conditions caused by spikeopathy.
(Biomedicines): ‘Spikeopathy’: COVID-19 Spike Protein Is Pathogenic, from Both Virus and Vaccine mRNA [LINK]
RELATED COURSES AT IPAK-EDU
The Biology of the Immune System - STARTING SOON JAN 2024
Aging Well: A Systems Biology Approach to Wellness for Older Children - STARTING SOON JAN 2024
RELATED
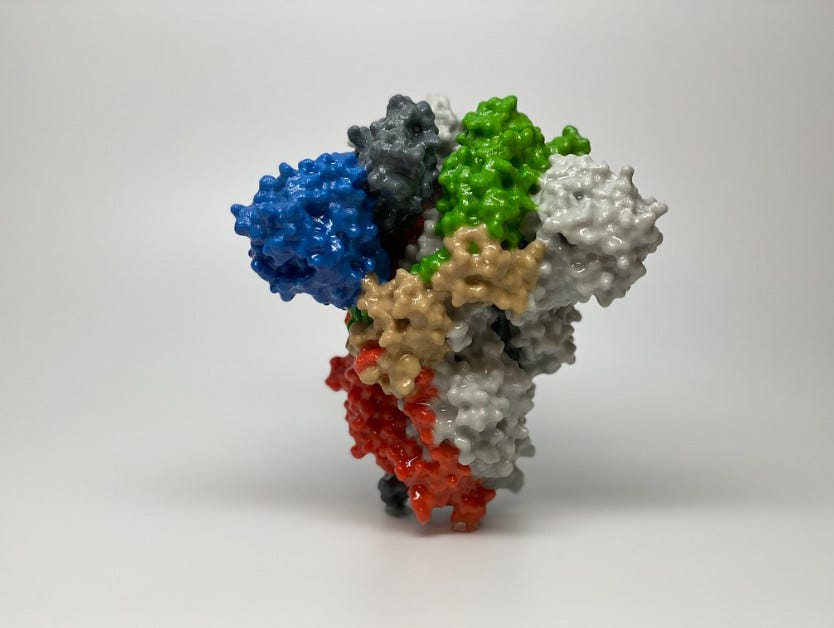
IMAGE CREDIT: US NIAID [SOURCE]. Used because our tax dollars paid for it.






I continue to be amazed & ever so thankful for your stellar approach, models, information & your ability to present this so a lay person can understand & grasp for the benefit of all. 🙌🫶👏
Yes James, the more jabs, the more entropy. Curiously, I believe teachers have a higher risk for cancer. My theory is that they are fighting bugs constantly. It would be interesting to compare HS teachers with say, K-3 teachers.