Hidden Burdens: Underdiagnosed Neuropsychiatric Symptoms in Autoimmune Disorders
The unseen intersection of autoimmunity and neuropsychiatry has implications for standards of care in both Autoimmune Disorders and Neuropsychiatric Care.
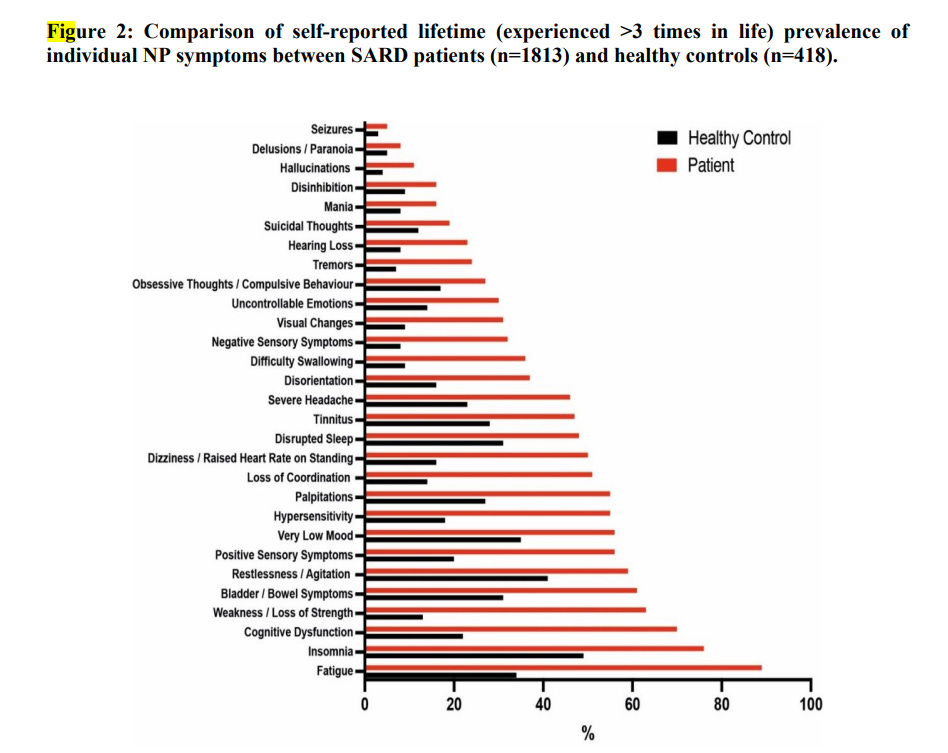
In an illuminating global study, researchers have found a higher prevalence of neuropsychiatric symptoms amongst patients suffering from systemic autoimmune rheumatic diseases (SARDs) than previously believed. This study, employing mixed methods, discovered these symptoms often go underreported, exacerbating the challenges of identification and treatment.
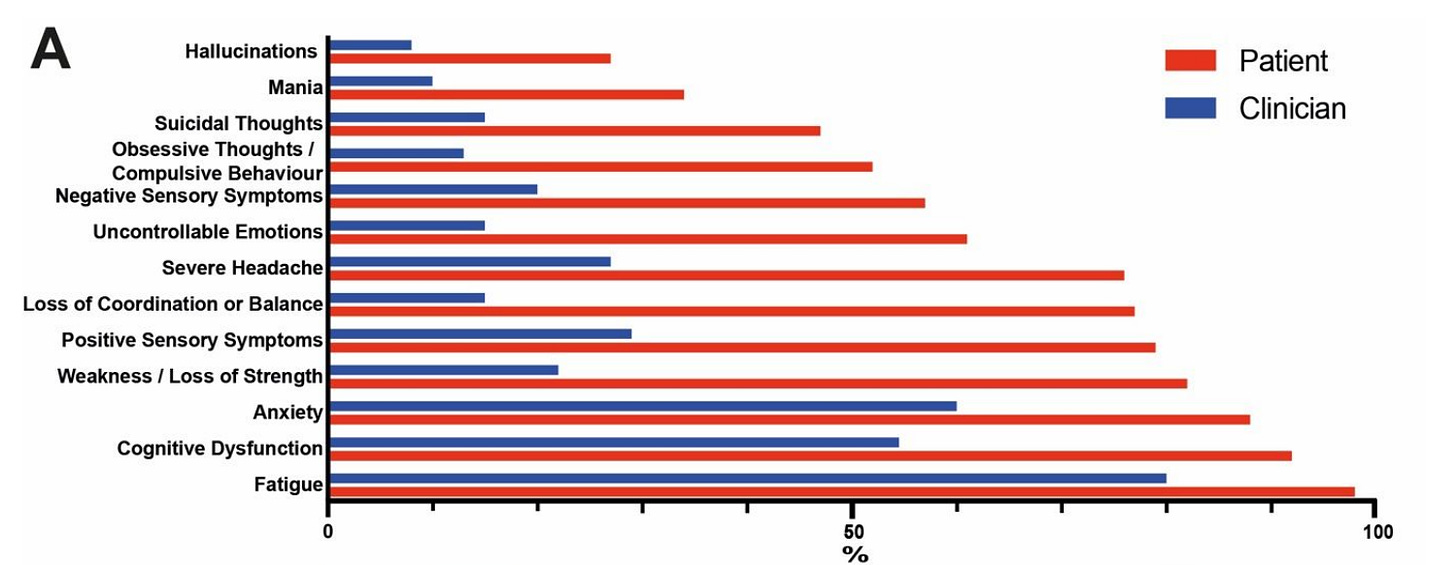
The research team, spanning international boundaries, surveyed both patients with SARDs and clinicians. The report found a higher incidence of neuropsychiatric conditions among patients with autoimmunity than persons without an autoimmune diagnosis. The report also exposed a considerable gap between the clinicians' and patients' understanding of these symptoms, often leading to underestimation or outright neglect of neuropsychiatric manifestations.
Fig 2 from the study.
The survey suggested that more than half of SARD patients seldom or never reported their neuropsychiatric symptoms to their healthcare providers. This discrepancy was attributed to patients being unaware of the wide array of potential neuropsychiatric symptoms and reluctance to disclose such symptoms due to perceived disbelief or disregard by clinicians.
Notably, the researchers uncovered higher instances of self-reported hallucinations amongst SARD patients, including those suffering from systemic sclerosis, vasculitis, and undifferentiated connective tissue disease (UCTD). This finding challenges the prevailing assumption that hallucinations are exclusive to SLE, commonly known as lupus, amongst the SARDs.
Fig 3A from the study.
The existing process of identifying SARD neuropsychiatric symptoms primarily relies on patient reporting and clinician judgement. This method presents significant concerns due to under-reporting and the highly varied prevalence estimates by clinicians. The study stresses the need for increased application of patient-reported outcomes measures (PROMs) for symptoms such as headache and fatigue that can only be assessed by the patient.
Moreover, the study identifies psychiatrists as vital assets to the healthcare team, due to their ability to empathetically elicit and value subjective reports. The inclusion of psychiatrists in patient care could enhance the identification of neuropsychiatric symptoms currently undetectable through objective tests.
The researchers urge for a revision of SARD guidelines and criteria, to incorporate greater consideration for neuropsychiatric symptoms. They believe this could be achieved through increased multidisciplinary international collaborative research.
Additionally, the study underscores the importance of including patients as equal collaborators in research, echoing EULAR (European League Against Rheumatism) guidance. Recognizing and utilizing patient knowledge could help minimize diagnostic errors and underestimations of neuropsychiatric manifestations.
While the research provides hope for improved SARD neuropsychiatric care, it also acknowledges the study's limitations, including potential recall bias, self-stated diagnoses, and non-representative sampling due to online survey recruitment.
The study highlights a greater and wider-ranging neuropsychiatric symptom burden in SARDs patients than previously recognized. It argues for more effective inter-disciplinary and patient-clinician collaboration to identify symptoms and design research that accurately reflects the experiences of SARD patients.
Consider signing up for related courses at IPAK-EDU for the fall semester!
Integrative Wellness for Mental Health - Kozek-Giustra
The Biology of Immunology - Lyons-Weiler
Psychology Made as Easy as 1, 2, 3 - Henriques
What does this mean for those suffering from autoimmune diseases and psychiatric disorders? The discovery underscores the profound intersection of physical and mental health. It places renewed importance on comprehensive, patient-centered care that addresses both the physiological and psychological aspects of chronic illness. A deeper understanding and acknowledgment of the neuropsychiatric burden in SARDs will lead to improved diagnosis, treatment, and patient outcomes. Thus, a step towards dismantling the artificial divide between physical and mental health, fostering a more holistic approach to patient care.
This international study carries significant implications for standards of care in both autoimmune diseases and neuropsychiatric disorders. The findings highlight critical gaps in understanding, diagnosing, and treating the neuropsychiatric manifestations of systemic autoimmune rheumatic diseases (SARDs). Here are the potential impacts:
1. **Holistic Care Approach**: The under-recognized and under-reported neuropsychiatric symptoms necessitate a more holistic approach to patient care, emphasizing the integration of mental health services in the treatment plans for patients with autoimmune diseases.
2. **Importance of PROMs**: The study underscores the value of Patient-Reported Outcomes Measures (PROMs) for capturing subjective symptoms, which often remain under-detected by objective diagnostic tests. This could prompt a shift towards routine use of PROMs in clinical settings to better understand and manage patient experiences.
3. **Role of Psychiatry in SARD Care**: The research illustrates the crucial role of psychiatry in the management of SARDs. Given their skill in empathetically eliciting and evaluating subjective reports, psychiatrists could enhance the recognition of neuropsychiatric symptoms and be instrumental in delivering comprehensive patient care.
4. **Revision of Clinical Guidelines**: The findings advocate for an update of existing SARD clinical guidelines and criteria, which currently may not adequately consider the neuropsychiatric symptoms. This calls for health organizations and governing bodies to reevaluate and revise standards of care to reflect the broad range of symptoms experienced by patients.
5. **Multidisciplinary Collaboration**: Given the complex and systemic nature of SARDs, effective management requires a multidisciplinary approach. The study calls for better clinical and academic collaboration between rheumatology, neurology, and psychiatry, to foster comprehensive care and further research into SARD neuropsychiatric manifestations.
6. **Patient Involvement in Care and Research**: The study highlights the importance of involving patients as equal collaborators in their care and in research. The unique insights of patients, which are currently underutilized, could enhance understanding of the disease, reduce diagnostic errors, and lead to innovations in care and treatment.
7. **Educational Programs**: The significant discrepancy between clinician and patient understanding of neuropsychiatric symptoms underscores the need for educational programs. These programs should aim to increase awareness amongst both patients and clinicians about the potential neuropsychiatric symptoms associated with SARDs.
Overall, the study proposes a paradigm shift in the approach towards SARDs and neuropsychiatric disorders, encouraging a more integrated and comprehensive care model that better serves the needs of patients.
Melanie Sloan and others, Prevalence and identification of neuropsychiatric symptoms in systemic autoimmune rheumatic diseases: an international mixed methods study, Rheumatology, 2023;, kead369, https://doi.org/10.1093/rheumatology/kead369





Sadly, it did not include the role of nutritional deficiencies in autoimmune disease or neurocognitive symptoms. Yes, an interdisciplinary approach would help a lot, you just need to include a low histamine diet trained dietitian who also knows about magnesium and vitamin D metabolism.
Also, regarding the under-reporting, the smart autoimmune patient may have learned to keep their mental health symptoms to themselves as medication is generally used and often dangerous rather than helpful.
The genetic injections positioned as Covid vaccines create autoimmunity by definition. The correlation of autoimmunity and neurological effects referred to in your post could explain at least partially what many people are noticing anecdotally. That is, an increase in: short tempers, angry behaviour, aggressive driving, cognitive dullness, etc. in the general population of heavily injected countries.