Pfizer-BioNTech Vaccine Booster Study "90% Reduction in Mortality" was Likely a Fluke Caused by Healthy User Bias: Hoeg et al.
NEJM letter to the editor reveals a fatal flaw in the study that actually plagues most vaccine studies.
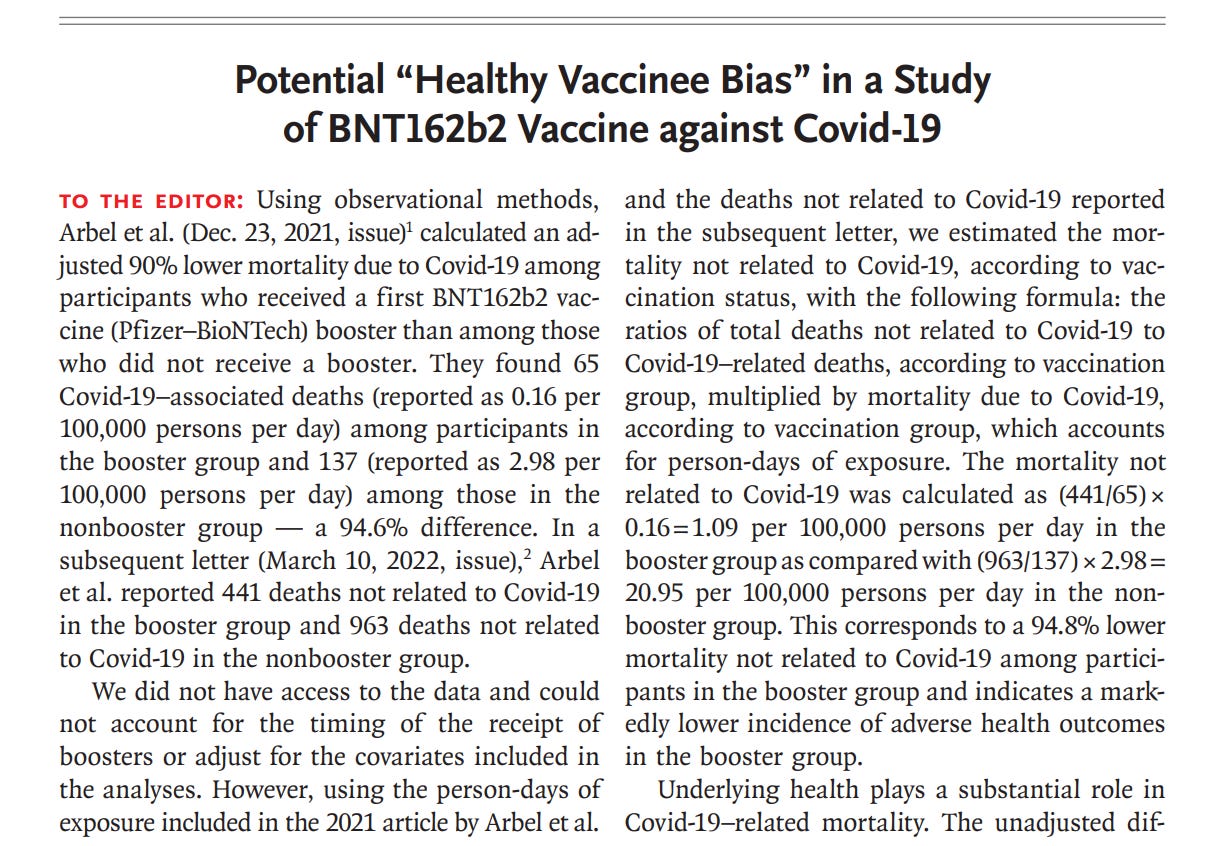
In a recent letter to the editor, Tracy Hoeg and colleagues reported on their analysis of Arbel et al. who, using observational methods, alleged that they found a significantly lower mortality rate due to Covid-19 among participants who received a Pfizer–BioNTech booster shot compared to those who did not. This result suggested that booster vaccination could have a major role in reducing the risk of death from Covid-19.
However, the authors of the response letter of July 20th raised concern about the validity of these findings. They calculated a similar reduction in mortality not related to Covid-19 in the booster group, which questions whether the vaccine booster is solely responsible for the reduced mortality. The authors suggests that healthy user bias may play a role – people who choose to get a booster shot might generally be more health-conscious, and thus healthier, than those who do not. This could potentially lead to an overestimate of the vaccine booster's effectiveness.
The authors stress that it is important to account for these factors to avoid skewed results, and they recommend including mortality not related to Covid-19 in all observational Covid-19 vaccine studies to provide a broader context.
This is a serious problem not just for the study, but also for public health policy: FDA based their policies on COVID-19 boosters on this potentially fatally flawed study (See Video by letter co-author Vinay Prasad, below). Hundreds of colleges still require their enrollees to abide by COVID-19 vaccine mandates, which is, of course, ludicrous given that every other sector of society has dropped the mandate requirement, including US healthcare workers and the US military.
Healthy User Bias a General Weaknesses of Observational Studies
While observational studies are an important tool in the field of epidemiology, they also have several weaknesses:
Confounding Factors: In observational studies, it is difficult to control for all the variables that may influence the outcome. For example, people who choose to get vaccinated or boosted might have different health behaviors or underlying health conditions than those who do not. This can create a “confounding bias”.
It is especially difficult to know when a potentially confounding variable is actually a confounding variable instead of a “co-predictor”. This is because the interaction terms between the main effect (vaccine exposure) and potential co-predictors are practically never studied in vaccine observational studies.
Healthy User Bias: This is a specific type of confounding where people who choose to get vaccinated are generally healthier and would therefore naturally have lower rates of illness or death. This can make the vaccine appear more effective than it really is.
Lack of Randomization: In a randomized controlled trial (RCT), participants are randomly assigned to either receive the treatment or not, which helps to control for confounding variables. However, observational studies lack this randomization, which can lead to bias.
Reliance on Self-reporting: Often, observational studies rely on participants' self-reporting, which can be unreliable or inaccurate.
Difficulty in Establishing Causality: Observational studies can show correlation, but they cannot definitively establish causality. This is because there might be unseen variables influencing the outcome. So, while we might see a lower death rate among those who got a booster shot, we cannot conclusively say that the booster shot is the cause of this reduced mortality.





Lol. "90% reduced mortality" yet we're seeing an astounding, unheard-of, 13 Sigma deviation in all cause mortality in the 0-24 age group (the group LEAST likely to suffer mortality), currently running in excess of 26%.
PFIZER LIES.
University of Michigan has Facebook ads for a research opportunity recruiting volunteers who declined the vaccine because they had previous allergic reactions to other vaccines, or who had an allergic reaction to an initial covid vaccine and therefore avoided further covid vaccine doses.
They recognize that those people are out there, and should realize that this fact can contribute to healthy user bias.