Mechanisms of Increased Oncogenesis and Increased Mortality in Cancer Related to SARS-CoV-2 Spike Protein mRNA Injections: Japan
Repeated Exposures Cause Increased Risk (#PathogenicPriming) in One Age Group so Far; Breast Cancer an Outlier
A study by Gibo et al. (2024) entitled Increased Age-Adjusted Cancer Mortality After the Third mRNA-Lipid Nanoparticle Vaccine Dose During the COVID-19 Pandemic in Japan, provides an analysis of the impacts of the COVID-19 pandemic, particularly the vaccination efforts, on cancer mortality in Japan.
The study examines age-adjusted mortality rates (AMRs) for various types of cancer during the COVID-19 pandemic, specifically looking at changes following the administration of the third dose of mRNA-lipid Nanoparticle injections.
The authors reported a distinct temporal pattern in cancer mortality rates.
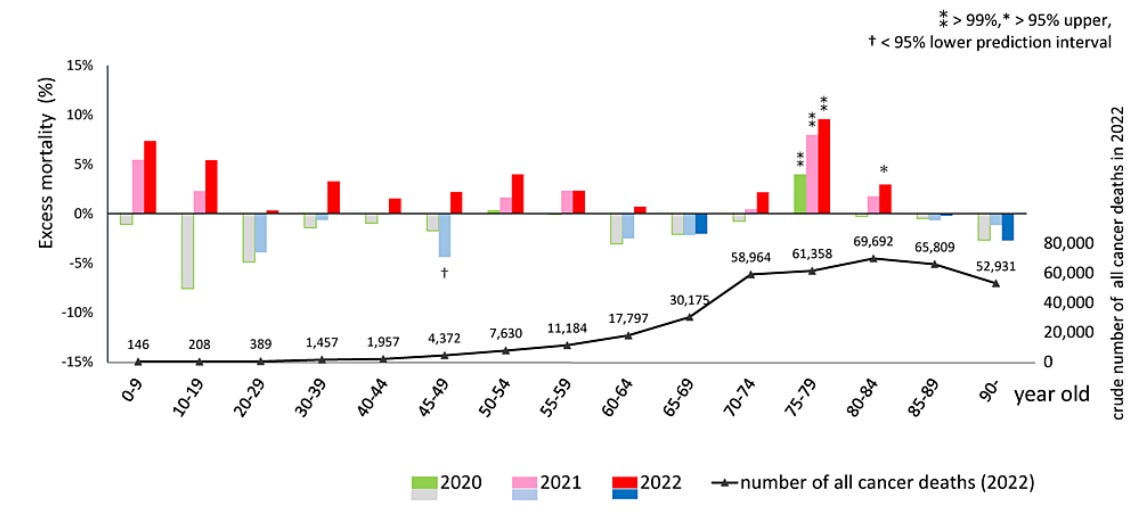
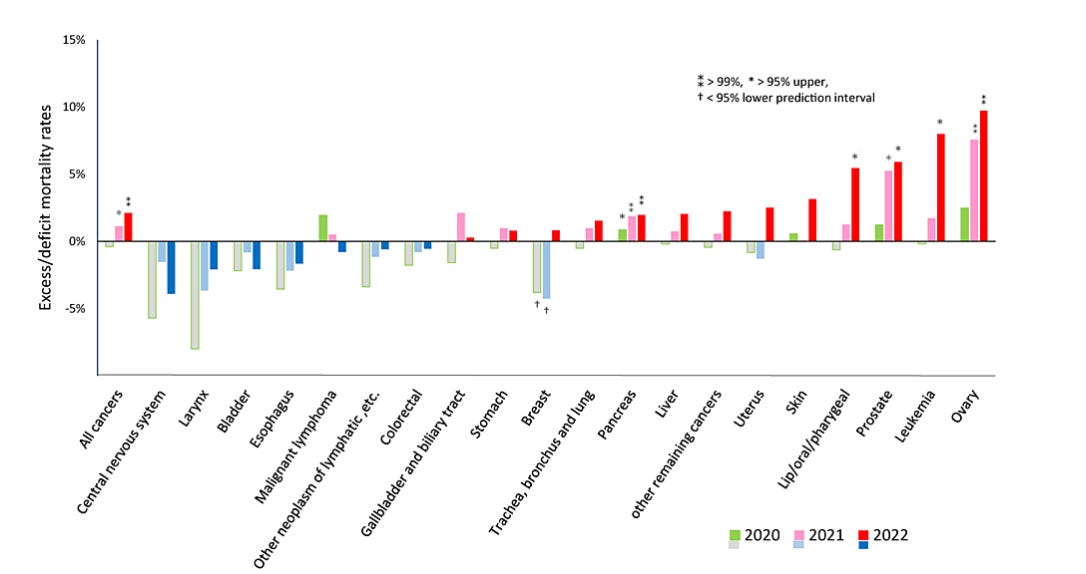
In 2020, there was no noticeable increase in cancer mortality, indicating that the initial phase of the pandemic did not significantly affect cancer death rates. However, following the rollout of the first and second doses of the COVID-19 vaccine in 2021, an increase in excess mortality for some cancer types was observed. This trend became more pronounced in 2022, after the administration of the third vaccine dose, where significant excess mortality was noted across all cancers, with particular increases in ovarian, leukemia, prostate, lip/oral/pharyngeal, pancreatic, and breast cancers.
The also study identified a slowdown in the decrease of age-adjusted mortality rates (AMRs) for the four most prevalent cancer deaths (lung, colorectal, stomach, and liver) in 2021 and 2022, suggesting a deceleration in the progress against these cancers during the later stages of the pandemic.
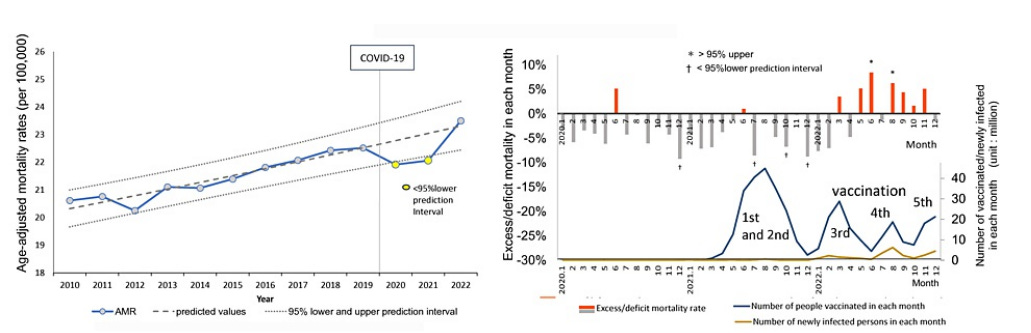
(Left Side) The blue line with markers shows the real number of deaths from cancer (adjusted for age) per 100,000 people. A dashed line shows what the authors predicted those numbers would look like based on past data. Dotted lines frame what would be considered normal fluctuations around that prediction. (Right Side) The bottom axis shows each month of the pandemic years (2020, 2021, 2022). Years where deaths were unusually high are marked: yellow spots mean slightly higher than expected, and pink spots mean much higher than expected. The left vertical axis tells us how much higher the actual deaths were compared to the percentage expected. The right vertical axis shows the number of COVID-19 vaccinations and the deaths caused by COVID-19.
In the study figure, a vertical line shows when COVID-19 started affecting Japan. Until 2020, the number of deaths decreased, but then it stopped decreasing. In 2021, deaths were higher than what is considered normal, and in 2022, they were even higher, going beyond the highest expected limit.
Deaths were way higher than expected, first in August 2021, around the same time many people were getting their first or second vaccine shots, and then in May 2022, after a lot of people received their third shot.
By Cancer Type in Detail
The study found that in 2020, only deaths from pancreatic cancer were slightly higher than what was normally expected. But as the years went on during the pandemic, more types of cancer showed unusually high death rates. In 2021, three out of twenty cancer types had higher deaths than expected, and by 2022, this number increased to five. The cancers with these higher death rates were ovarian cancer, leukemia, prostate cancer, lip/oral/pharyngeal cancer, and pancreatic cancer, with ovarian cancer showing the largest increase.
For ovarian cancer, the number of deaths was about 7.6% higher than expected in 2021 and increased to 9.7% higher in 2022. Leukemia, prostate cancer, lip/oral/pharyngeal cancer, and pancreatic cancer also saw increases, with leukemia deaths 8% higher than expected in 2022 and similar rises in the other types.
Interestingly, breast cancer showed a decrease in deaths compared to what was expected in 2020 and 2021. However, in 2022, there was a slight increase in breast cancer deaths, but this change was not large enough to be considered statistically significant. This means that while there was an uptick in breast cancer deaths in 2022, the numbers could still be due to random chance rather than a definitive increase.
The ovarian cancer signal is striking:
The other cancers show similar trends.
Breast cancer has a different pattern:
Mechanisms Cited
The mechanisms cited in the study regarding the potential impacts of mRNA-LNP vaccines on cancer mortality and development are complex, citing various mechanisms of oncogenesis, many of which have been discussed here on Popular Rationalism many times before:
Vaccine Distribution and Molecular Concentration: The authors report that the number of mRNA molecules per vaccine dose is extremely high, ranging into the trillions. According to the authors, there are only about 3 times more cells in the human body than LNPs. Once injected, these vaccines are distributed widely across the body, including critical organs like the liver and ovaries.
Spike Protein Production: The vaccines lead to the production of the COVID-19 spike protein, which remains in the body for months. This is much longer than the spike protein from the virus itself, which typically disappears within a few weeks after infection.
Thrombosis Risk in Cancer: Cancer increases the risk of blood clotting. The spike protein and the vaccine's lipid nanoparticles (LNPs) might further raise this risk, potentially explaining higher mortality rates in cancer patients after vaccination.
Immune System Impact: The vaccines suppress important parts of the immune system that usually help detect and destroy cancer cells. This could weaken the body's natural defenses against cancer.
The authors report that following mRNA vaccination, cells that produce large amounts of SARS-CoV-2 spike protein (S-protein) also release exosomes filled with specific microRNAs (miRNAs), particularly miRNA-148a and miRNA-590. These miRNAs target and suppress the activity of the ubiquitin-specific peptidase 33 (USP33) and interferon regulatory factor 9 (IRF9) pathway in microglia, which then take up these exosomes. This suppression leads to a decrease in the function of type I interferons (IFN) and BRCA2, both essential for combating cancer cells by enhancing immune surveillance and DNA repair mechanisms, respectively.
Moreover, the presence of the S-protein seems to enhance the expression of programmed death-ligand 1 (PD-L1) across various immune and tumor cell types, as well as programmed cell death protein 1 (PD-1) on T cells. This upregulation impairs the effective functioning of CD4+ and CD8+ T cells, crucial players in the body's defense against malignancies, by promoting an immunosuppressive environment within tumors. This mechanism further hampers the immune system's ability to surveil and eliminate cancer cells, potentially contributing to an increased risk or progression of cancer following vaccination.
Inflammation and Autoimmune Reactions: The vaccines can, via pathogenic priming, trigger autoimmune reactions, where the body mistakenly attacks its own cells. This can be particularly dangerous if the tissues attacked are immune cells and proteins.
Interaction with Cancer-Related Genes: The spike protein may interfere with genes crucial for repairing DNA damage, such as BRCA1, BRCA2, and P53. This interference could increase the risk of cancer or worsen existing cancers.
Hormone Receptor Sensitivity: Certain cancers are sensitive to hormones. The spike protein can bind to hormone receptors, potentially driving the growth of hormone-sensitive cancers like breast and ovarian cancer.
Activation of Latent Viruses: The vaccine-induced immune response might accidentally reactivate latent viruses associated with certain cancers, contributing to cancer development or progression.
Vaccine mRNA Integration: mRNA can be reverse transcribed into DNA and become integrated into the human genome, potentially causing genetic mutations that increase cancer risk.
Reduced Screening. In Japan, during 2020, there was a notable drop in the number of people getting checked for stomach, lung, colorectal, breast, and uterine cancers by about 24.4% in community health settings, although workplace screenings barely changed, decreasing by just 0.9%. By 2021, the number of these important cancer screenings started to go back to the usual rates seen before the pandemic. The decrease in cancer screenings and overall healthcare services during the lockdown might have led to an increase in deaths from various types of cancer. However, this reduction in healthcare access does not fully explain the significant rise in death rates observed for six specific types of cancer.
The authors conclude that more research is needed to discern which mechanisms are in play. They may all be factors, or some may be more important than others in different cancer types.
THE STUDY: Gibo M, Kojima S, Fujisawa A, et al. (April 08, 2024) Increased Age-Adjusted Cancer Mortality After the Third mRNA-Lipid Nanoparticle Vaccine Dose During the COVID-19 Pandemic in Japan. Cureus 16(4): e57860. DOI 10.7759/cureus.57860







Best to learn about fenbendazole (safe, effective, inexpensive, OTC) medicine for cancer treatment now and not under the stress of a diagnosis of self or loved one https://fenbendazole.substack.com
According to the authors, there are only about 3 times more cells in the human body than LNPs.
That is roughly true for Pfizer (12 trillion); however, Moderna contains 40 trillion which is more than the approx. 36 trillion cells in the human body. And, only 4 trillion of those cells are nucleated:
https://evolutionaryhealthplan.info/#_Ref83404023