Lyons-Weiler Responds to Hotez
The vaccine activists who conducted and promoted science-like activities to hide vaccine risk are acting as though we don't know about the fraud.
Hotez believes that telling the world that there will be four years of “anti-vaccine activism” is an effective Public Health message. In reality, Robert F. Kennedy Jr’s appointment will mean an end to narrative enforced “science-like activities” and a return to bona fide science. We’re planning four years or more of objective science conducted on vaccines. And we are planning prosecutions for fraud, misuse of federal research funding, all of it. As long as he continues to attempt to gaslight with these tropes, we will not be able to take him, or people who act like him, seriously.
Mischaracterizing Vaccine Risk Awareness
In It Won’t End with COVID: Countering the Next Phase of American Antivaccine Activism 2025–29, published this week in PLOS One, Peter Hotez begins by framing all vaccine skepticism as an ideological phenomenon, driven by political partisanship and disinformation campaigns. This reductive view is not only misleading but also entirely counterproductive. It ignores the legitimate, evidence-based concerns raised by a massive number of individuals and groups, many of whom describe themselves as vaccine risk-aware. By dismissing these concerns as “antivaccine activism” or “hesitancy,” Hotez fails to address the complexity and diversity of the movement. There is a spectrum of positions in the community he casts as “antivaccine”, but he seeks to alienate and minimize those who have sought dialogue and reform rather than confrontation. He seems to be succeeding at increasing the risk of alienating himself from the future of science.
The Problem with Oversimplification
Hotez’s use of terms like vaccine hesitancy and antivaccine is both scientifically imprecise and rhetorically polarizing. These terms suggest that individuals questioning vaccine policies are either indecisive or fundamentally opposed to vaccination, ignoring the nuanced positions many hold. For instance, vaccine hesitancy implies that individuals are simply delaying vaccination due to uncertainty, whereas antivaccine paints them as ideological opponents to all immunizations. Neither term captures the concerns of those actively examining vaccine safety, efficacy, and ethical issues.
The failure to differentiate between legitimate critique and ideological opposition has significant consequences. It is an attempt to delegitimize the voices of scientists, medical professionals, and informed citizens who challenge the status quo based on data and firsthand experiences. It also discourages public health personnel from engaging with these voices constructively, perpetuating a cycle of mistrust.
The Diversity of Vaccine Risk Awareness
The vaccine risk awareness movement is far from a monolithic group of ideological nutjobs. It encompasses a broad spectrum of individuals and motivations, united by a shared concern for safety, transparency, and ethical medical practices. Among them are:
Parents who, after observing adverse events in their children post-vaccination, seek greater accountability and assurance of safety in the vaccination process. Some of these parents then reject vaccines outright, other do not. But all are demanding answers to why adverse events occur and how they can be prevented because, as they have said, they would not anyone to have experience what they had to endure. The deserve to be treated with utmost respect.
Researchers, Scientists and Doctors who have found and have highlighted methodological flaws in vaccine safety studies, such as the lack of true placebos, short follow-up periods, and conflicts of interest. Their critiques are rooted in scientific rigor and a commitment to improving public health outcomes. Many merely want to promote objectivity in science, and they have found that the vaccine risk aware public agrees, entirely, that fraud, not science, lies at the base of the issues of what is known about vaccines.
Advocates for Medical Ethics and Human Rights who oppose coercive mandates that undermine the principle of informed consent. These individuals emphasize the importance of personal autonomy and the right to make medical decisions free from undue pressure or societal shaming.
Concerned Citizens who question the integrity of public health institutions after observing inconsistencies, omissions, or manipulations in the communication of vaccine safety and efficacy.
This diversity of perspectives underscores the need for a more inclusive and nuanced approach to addressing vaccine-related concerns. Labeling all critiques as "antivaccine" not only oversimplifies the issue but also alienates people who might otherwise support vaccination if their questions and concerns were addressed transparently.
Hotez’s Missed Opportunity for Constructive Engagement
By failing to recognize the legitimacy of vaccine risk awareness, Hotez has missed an important opportunity to engage constructively with the future leaders of science in America. Instead of fostering dialogue, his approach perpetuates an "us versus them" mentality, further polarizing public health discourse. The polarizing tools - such as characterizing vaccine risk awareness as something that only exists on the “far right” - has nearly torn our society in two. Constructive engagement will require acknowledging the validity and value of certain critiques and working collaboratively to address them. For example:
Addressing parental concerns about adverse events by improving post-market surveillance systems and ensuring that these systems capture a broader spectrum of potential risks (e.g., making reporting vaccine injuries mandatory with penalties to doctors who fail to report; studies using whole-outcome awareness).
Responding to scientific critiques by conducting independent, transparent studies with robust methodologies that include true placebo groups and long-term follow-up.
Upholding the principle of informed consent by ending coercive mandates and providing clear, unbiased information about vaccine risks and benefits.
Being forthright on the realities of quantifiable risk; end biased messaging and stop burying vaccine injury risk under the unquantified euphemism of “rare”.
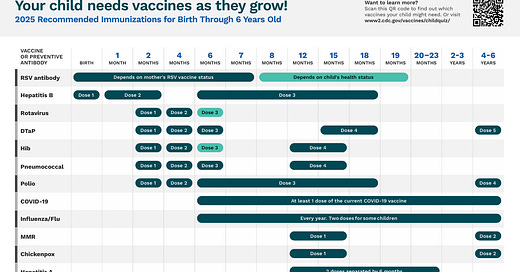
Here’s an example of biased messaging from the CDC webpage for the dense schedule from 0-6 years:
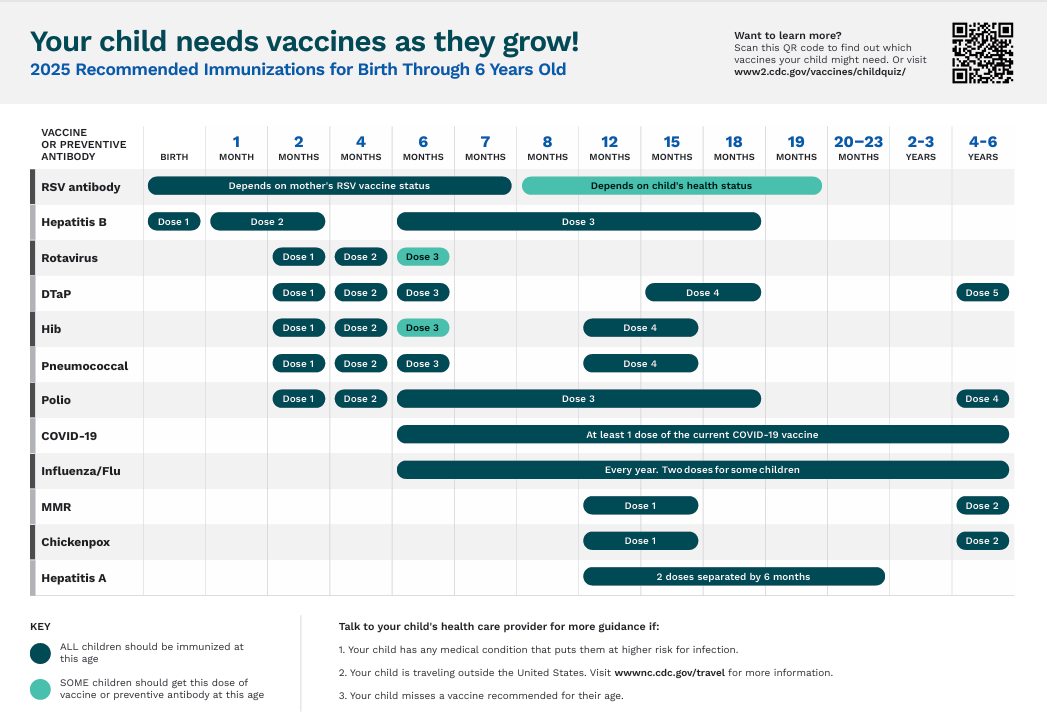
Further down the page, we see
What we do NOT see here is any attempt at quantifying the risk of these complications in 2025, nor a list of potential side effects and their quantified risk.
In fact, no where on these pages for the vaccine schedules for adults and children is the public made aware of any vaccine risks.
Thus, the messaging is biased: it leads web travelers to believe that the only risk involved is the risks associated with the disease. Risk consideration is not impossible; it is not even difficult if the CDC did their job right. I once calculated that children had a higher risk of dying traveling to and from the pediatrician’s office from a car accident than from COVID-19.
Such measures would not only address the concerns of vaccine risk-aware individuals but also regain trust in public health institutions, which has been significantly eroded by dismissive and polarizing rhetoric.
The Consequences of Misrepresentation
Hotez’s failure to accurately characterize vaccine risk awareness has broader implications for public health. By dismissing legitimate concerns as “antivaccine activism,” he undermines the credibility of public health messaging and alienates those seeking genuine reform. This approach risks driving individuals further away from centralized public health and fostering a sense of disenfranchisement among those who feel their voices are ignored. They are the most important and most relevant stakeholders at the table.
Moreover, the misrepresentation of vaccine risk awareness as purely ideological obscures the systemic issues within vaccine safety research and policy that must be addressed. It allows public health personnel to deflect accountability and avoid necessary reforms, perpetuating the very problems that fuel skepticism and mistrust.
A Path Toward Constructive Dialogue
The first step in addressing the concerns of vaccine risk-aware individuals is to acknowledge their legitimacy and diversity. Public health discourse must move beyond simplistic labels and engage with critiques in a transparent and respectful manner. This requires:
Recognizing the distinction between ideological opposition and evidence-based critique.
Creating platforms for dialogue where concerns can be raised and addressed without fear of dismissal or vilification.
Committing to reforms that prioritize safety, transparency, and informed consent.
By adopting these measures, public health personel might have a chance to regain trust and foster a more collaborative relationship with the public. Vaccine risk awareness is not an obstacle to progress, but an opportunity to strengthen the scientific and ethical foundations of vaccination policies.
Ethical Failures in Vaccine Policy
Ethical considerations are at the core of modern medicine, yet Peter Hotez’s framing of vaccination as a moral imperative often sidesteps critical questions about autonomy, consent, and the balance between individual rights and collective welfare. Vaccine policies, particularly those reliant on mandates and societal pressure, risk undermining the foundational principles of medical ethics and biomedical research ethics. This section will explore the failures of current vaccine policies to uphold informed consent and balance public health goals with respect for individual autonomy.
Informed Consent: A Foundational Principle
Informed consent is a cornerstone of ethical medical practice. It ensures that individuals are provided with clear, accurate, and comprehensive information about any medical intervention, including its risks, benefits, and alternatives. For consent to be truly informed, individuals must have the autonomy to accept or decline treatment without coercion. However, many vaccine policies fall short of this standard, as they increasingly rely on mandates, incentives, or societal shaming to drive compliance.
The principle of informed consent is particularly critical for vaccines, as they are administered to healthy individuals for preventive purposes. This inherently raises the bar for safety and transparency. Coercive practices, whether through employment requirements, school mandates, or public campaigns that vilify dissent, directly conflict with the voluntary nature of consent. These measures erode trust in public health institutions, as individuals perceive their autonomy as being overridden for collective benefit.
One glaring issue is the lack of full disclosure regarding vaccine risks. Package inserts and official communications often present risks as rare without providing meaningful context or acknowledging gaps in safety data. For example, the absence of long-term studies on certain vaccine components, such as adjuvants, is rarely discussed, leaving individuals unable to make fully informed decisions. By failing to provide a balanced and transparent account of risks and benefits, vaccine policies undermine the ethical requirement for informed consent.
Coercive Public Health Practices
Hotez’s framing of vaccine refusal as a moral failing feeds into a broader culture of coercion in public health. This culture is characterized by practices that pressure individuals into compliance rather than addressing their concerns through dialogue and evidence. These practices include:
Mandates: Laws requiring vaccination as a condition for attending school, employment, or participating in public life restrict individual choice and disproportionately affect those who question vaccine safety. While proponents argue that mandates protect public health, they often neglect to consider their impact on personal autonomy and trust.
Social Shaming: Public campaigns that vilify vaccine skeptics or risk-aware individuals contribute to societal polarization. By framing dissent as irrational or dangerous, these campaigns discourage open dialogue and alienate those with legitimate concerns.
Incentives and Penalties: Programs that offer financial incentives or impose penalties for non-compliance, such as withholding public benefits, further erode the voluntary nature of consent. These measures disproportionately impact marginalized populations, raising questions about equity and justice in public health policy.
The reliance on coercion not only undermines ethical principles but also risks backfiring. Individuals who feel coerced are more likely to resist or distrust public health initiatives, fueling skepticism and opposition. A more effective approach would prioritize engagement, transparency, and respect for individual autonomy.
Since vaccine safety relies on post-market surveillance, every person vaccinated has been enrolled in an uncontrolled human subjects study without free, prior and informed consent. Coercion is illegal under the Code of Federal Regulations. Seven years ago, this argument led to the release of a then-jailed mom Rebecca Bredow in Michigan (See FREE REBECCA BREDOW - END HER UNLAWFUL IMPRISONMENT NOW!). I hand delivered the petition to the Michigan judge who wrongfully imprisoned Rebecca after have the order to vaccinate her son James delivered to the wrong lawyer. Rebecca was released early, ostensibly for “good behavior”.
Balancing Public Good and Individual Rights
The tension between public health goals and individual rights is a longstanding ethical dilemma. Vaccination policies often invoke the concept of herd immunity to justify mandates, arguing that individual choices must sometimes be overridden to protect the vulnerable. While this argument has merit, it cannot be used to disregard individual autonomy entirely.
Balancing public good and individual rights requires a nuanced approach that respects both. This involves acknowledging that individuals are not clones, and have diverse risk tolerances and perspectives on medical interventions. Public health policies should provide options that accommodate these differences rather than imposing one-size-fits-all solutions. For example:
Offering exemptions for individuals with genuine safety concerns or medical contraindications ensures that policies remain inclusive and respectful.
Creating pathways for individuals to access detailed safety and efficacy data allows for more informed decision-making.
Engaging in community dialogue to address concerns and build trust fosters voluntary compliance rather than resistance.
Hotez’s approach, which emphasizes mandates and dismisses dissent as dangerous, risks deepening divisions and undermining public health. A more ethical framework would empower individuals to make informed choices while ensuring public health goals are pursued transparently and collaboratively.
Rebuilding Ethical Foundations in Public Health
Public health personnel must prioritize informed consent and voluntary participation to restore the ethical integrity of vaccine policies. This requires:
Transparent Communication: Providing comprehensive and balanced information about vaccine risks, benefits, and alternatives in accessible formats. This includes addressing gaps in safety data and acknowledging uncertainties honestly.
Ending Coercion: Shifting away from mandates, incentives, and penalties toward policies that respect individual autonomy and encourage voluntary participation.
Equal Protection: Ensuring that vaccine policies do not disproportionately burden individuals and families at special risk of vaccine injury or death due to vaccination.
Fostering Dialogue: Creating platforms for individuals to raise concerns, share experiences, and engage in constructive conversations with public health personnel.
Ethical public health policies must respect individual rights, even when pursuing collective benefits. By embracing transparency and accountability, public health could have a chance to regain trust and foster a more collaborative relationship with the communities it serves.
Gaps in Vaccine Safety Research
Peter Hotez’s confidence in vaccine safety reflects a troubling disregard for the significant gaps in vaccine safety research. The scientific foundations of safety assessments remain incomplete and, in some cases, deeply flawed. These gaps include methodological weaknesses in pre-licensure trials, inadequacies in post-market surveillance, and unresolved questions about specific vaccine components such as adjuvants. Public health personnel risk undermining the trust they seek to build by failing to address these shortcomings.
Pre-Licensure Trial Limitations
By design, vaccine trials focus on detecting acute adverse events, often neglecting long-term outcomes. The typical follow-up periods for pre-licensure trials range from weeks to months, insufficient to identify delayed adverse effects such as autoimmune or neurological disorders. This limitation is particularly concerning for vaccines administered to children, whose developing immune and neurological systems may exhibit unidentified vulnerabilities.
Another critical flaw in pre-licensure trials is the frequent use of active controls rather than true placebos. For example, trials may compare a new vaccine to an older vaccine or an adjuvant-containing solution instead of a saline placebo. This practice obscures the detection of adverse events unique to the new vaccine, as any shared risks with the control are effectively normalized. The result is a skewed safety profile that can fail to capture meaningful differences.
Conflicts of interest further erode the credibility of pre-licensure research. Vaccine manufacturers sponsor the majority of trials, raising questions about bias in study design, data interpretation, and reporting. Independent replication of trial results is rare, leaving gaps in the evidence base that are critical for comprehensively assessing safety and efficacy.
The Role of Adjuvants: Aluminum Under the Microscope
Adjuvants like aluminum are used to enhancing immune responses in certain vaccines and save money on antigen use. However, their safety profiles remain insufficiently studied. Aluminum has long been used in vaccines, but its biological effects raise serious questions:
Induction of Autoimmunity: Aluminum is used in animal models to induce autoimmune diseases for drug development studies. This demonstrates its capacity to disrupt immune tolerance, yet similar mechanisms in humans are poorly understood.
Persistence in the Body: Research shows that aluminum adjuvants can accumulate in lymph nodes and travel to the brain, raising concerns about neurotoxicity and chronic inflammation.
Lack of Comparative Studies: Despite these concerns, there is a paucity of research comparing aluminum-adjuvanted vaccines to those without adjuvants or using alternative adjuvants like calcium phosphate. This leaves a critical gap in understanding the relative risks and benefits of adjuvant use.
The continued reliance on aluminum without comprehensive safety assessments reflects a broader pattern of insufficient attention to vaccine components. Addressing these concerns requires transparent, independent research that examines both the short- and long-term effects of adjuvants.
Post-Market Surveillance: A Flawed Safety Net
Post-market surveillance is often presented as a safety net for identifying rare or long-term adverse events, but its limitations undermine its effectiveness. Systems like the Vaccine Adverse Event Reporting System (VAERS) depend on voluntary reporting, which captures only a small fraction of actual adverse events. Studies estimate that fewer than 10% of adverse events are reported, creating significant underreporting biases.
Even when adverse events are reported, the methods used to analyze them often fail to establish causality. Observational studies frequently rely on arbitrary inclusion or exclusion of variables, diluting associations between vaccines and adverse events. This practice, known as "data dredging," is a form of statistical manipulation that can obscure meaningful safety signals. For example, significant associations between vaccines and neurological conditions have often been reanalyzed repeatedly until statistical significance disappears, effectively dismissing concerns without addressing the underlying data transparently.
The result is a post-market system that is reactive rather than proactive, relying on passive signals instead of active monitoring. This approach not only delays the identification of potential safety issues but also undermines public trust when adverse events are dismissed without clear explanations.
Suppressing Safety Signals: Historical Lessons
History provides numerous examples of vaccine safety signals being ignored or suppressed, often with dire consequences:
Cutter Incident: In the 1950s, faulty batches of polio vaccine caused paralysis in hundreds of children. Initial warnings were dismissed until the scale of harm became undeniable. Photos of Cutter Incident victims have been used to promote polio vaccination.
H1N1 Narcolepsy Cases: The Pandemrix vaccine, used during the 2009 H1N1 pandemic, was linked to narcolepsy in Europe. Despite early reports of adverse events, it took years for regulators to acknowledge the association.
Aluminum in HPV and other Vaccines: Persistent safety concerns about aluminum-containing HPV and other vaccines have been downplayed, even as independent research has established links to autoimmune conditions due to exposure to vaccine-type aluminum.
These cases highlight the dangers of prematurely dismissing safety concerns and underscore the need for robust, transparent safety monitoring systems.
Toward a More Comprehensive Safety Framework
Closing the gaps in vaccine safety research requires a paradigm shift in assessing and monitoring safety. This includes:
Independent Studies: Funding independent, placebo-controlled studies to evaluate both short- and long-term safety profiles of vaccines and their components.
Active Monitoring Systems: Transitioning from passive systems like VAERS to active surveillance programs that capture real-time safety data.
Transparency and Data Sharing: Ensuring that raw trial data and post-market findings are publicly accessible for independent review.
Comparative Adjuvant Studies: Investigating the relative safety of different adjuvants and exploring alternatives to aluminum.
By addressing these gaps, public health personnel may be able to regain trust and ensure that vaccine policies are grounded in robust, independent evidence. The failure to confront these issues transparently only perpetuates skepticism and undermines the very goals of vaccination campaigns.
Real-World Effectiveness vs. Controlled Trial Efficacy: The Translational Failure of Vaccines
Peter Hotez’s article assumes that vaccines’ apparent success in controlled trials translates seamlessly into real-world effectiveness, but this assumption overlooks the complexities of large-scale implementation. While controlled trials often show high efficacy under ideal conditions, real-world outcomes can diverge significantly due to factors such as waning immunity, breakthrough infections, failure to assess efficacy and safety across representative groups, and the challenges of co-administration. By failing to address these issues, Hotez presents an overly simplistic narrative that undermines public trust and fails to account for the multifaceted nature of vaccine deployment.
From Trials to Reality: The Efficacy-Effectiveness Gap
Controlled trials are test a vaccine’s ability to prevent specific outcomes, such as infection or severe disease, under carefully controlled conditions. These trials often exclude high-risk populations, such as individuals with pre-existing conditions or those taking multiple medications, to reduce variability and focus on the vaccine’s core efficacy. While this methodology is scientifically rigorous, it creates a gap between trial results and real-world effectiveness.
In the real world, vaccines are administered to diverse populations with varying health statuses, genetic backgrounds, and environmental exposures. These factors can influence how well a vaccine performs in the general population after FDA approval or CDC recommendation, leading to outcomes that differ significantly from those observed in trials. I call this translational failure, and it is an important concept in translational research that must be adopted as a central concern for all of biomedical progress. For example:
Waning Immunity: Many vaccines, such as those for COVID-19 and pertussis, show a decline in immunity over time. This waning immunity necessitates frequent booster doses, which can strain public health systems and lead to lower compliance rates.
Breakthrough Infections: Even in highly vaccinated populations, breakthrough infections occur, challenging the narrative that vaccines provide near-total protection. This phenomenon is particularly evident with rapidly mutating pathogens like influenza and SARS-CoV-2.
Negative Efficacy: Emerging data suggest that certain vaccines, under specific conditions, may increase susceptibility to variants or other unintended outcomes. For example, some studies have indicated that mRNA COVID-19 vaccines may exhibit negative efficacy against newer variants after repeated doses.
Population-level variation in responses to vaccines. Age, sex, comorbidities, and socioeconomic status can influence vaccine effectiveness. For example, older adults and immunocompromised individuals often exhibit weaker vaccine responses, requiring tailored strategies beyond a one-size-fits-all approach.
Adverse events not seen in the clinical trials. When attempts are made to minimize, via study design or data analysis, the discovery of adverse events to drugs or vaccines that might have widespread use, public health will suffer. Science is said to be self-correcting, but in this regard, we have only seen the practice proliferate unchecked. Fauci and Collins argued that Phase 2 and Phase 3 trials of COVID-19 vaccines should be combined; this prevented the validation by replication of adverse key events that could be been warned about.
It’s not not adverse events that are biased. Both Moderna and Pfizer grossly over-estimated efficacy in the early clinical trial by not counting cases, hospitalizations, and deaths until five, and then eight weeks after the initial dose of the mRNA jabs. This bias, called the Lyons-Weiler/Fenton effect, or case window counting bias, must never be allowed to be repeated. See articles on PopularRationalism.Substack.Com.
Attempts to bias estimates of efficacy and adverse events must be criminalized and fines and sentences levied against the perpetrators. These discrepancies highlight the need for ongoing intensive scrutiny and monitoring vaccination strategies to better reflect real-world conditions.
Waning Immunity and Breakthrough Infections
Waning immunity is a well-documented phenomenon for many vaccines, yet public health messaging often fails to address it transparently. For example:
Pertussis Vaccines: Acellular pertussis vaccines replaced whole-cell versions due to safety concerns, but they provide shorter-lived immunity. This has contributed to periodic outbreaks even in highly vaccinated populations.
MMR (Mumps): Outbreaks of mumps in highly and fully vaccinated populations have revealed that the mumps virus component of the MMR is becoming ineffective.
COVID-19 Vaccines: Studies have shown that immunity from mRNA vaccines declines within months, necessitating booster doses. However, booster campaigns often face logistical challenges and lower uptake rates compared to initial doses.
Breakthrough infections further complicate the narrative. While vaccines can reduce the severity of illness, their ability to prevent transmission or infection is not absolute. This limitation is particularly significant for pathogens like SARS-CoV-2, where variants with immune-escape capabilities can spread even in highly vaccinated populations. Public health messaging that overemphasizes protection against transmission risks eroding trust when real-world outcomes fail to align with expectations.
The Complexity of Negative Efficacy
Perhaps the most contentious issue in vaccine effectiveness is the potential for negative efficacy, where vaccinated individuals become more susceptible to specific outcomes. For example:
Dengue Vaccine: The Dengvaxia vaccine increased the risk of severe dengue in individuals who had not been previously exposed to the virus, leading to fatalities and public outcry.
COVID-19 Vaccines: Repeated mRNA vaccine doses may reduce protection against certain variants, raising questions about optimal dosing strategies.
Pathogenic Priming: Chronic illness due to repeated immune activation to epitopes similar to human proteins can lead to chronic illness and strange, diffuse, hard-to-diagnose syndromes that are not sufficiently studied. Symptoms like these are dismissed during early first-in-human clinical trials based on medical opinion by physicians employed by the vaccine manufacturers- without the benefit of the science needed to assess causality. Autoimmunity against human proteins can lead to chronic illness; autoimmunity againt immune proteins can be expected to cause immune deficiency and negative efficacy.
Negative efficacy challenges the assumption that more vaccination is always better and underscores the need for nuanced, evidence-based approaches to vaccine policy.
Toward a More Realistic Assessment of Effectiveness
Addressing the gap between controlled trial efficacy and real-world effectiveness requires a more transparent and adaptive approach to vaccination policy. This includes:
Enhanced Surveillance Systems: Monitoring vaccine performance in diverse populations to identify factors influencing effectiveness.
Co-Administration Studies: Conducting rigorous research on the combined effects of multiple vaccines to optimize schedules and minimize risks.
Tailored Strategies: Developing targeted vaccination approaches for high-risk groups, such as older adults or individuals with comorbidities.
End Analysis-to-Result: Retrospective studies designed to fail to detect adverse event associations via repeated analyses and arbitrary model selection must end. Developing and using prediction science to predict who is at risk—and get them out of harm’s way—is far more ethical on the balance of risk management. We must replace risk perception management with bona fide risk management.
Honest Communication: Providing balanced public health messaging that acknowledges limitations and uncertainties while highlighting the benefits of vaccination.
Bridging the Gap
Hotez’s failure to address the complexities of real-world vaccine effectiveness reflects a broader problem in public health discourse. By focusing exclusively on controlled trial results, he presents an incomplete picture that risks undermining public trust. A more realistic assessment of vaccine performance, grounded in transparency and adaptability, is essential for earning confidence and ensuring a viable future for public health.
Disinformation vs. Legitimate Critique
Peter Hotez frames dissent against vaccine policies as disinformation, dismissing critiques as ideologically driven and factually baseless. This framing is not only inaccurate but also counterproductive. By conflating legitimate scientific and ethical concerns with misinformation, Hotez undermines the credibility of public health messaging and stifles constructive dialogue. A more nuanced approach is essential—one that distinguishes between genuine critique and outright falsehoods while fostering transparency and accountability.
The Danger of Conflating Critique with Disinformation
Labeling all vaccine skepticism as disinformation oversimplifies a complex issue and alienates those with valid concerns. Legitimate critiques often stem from gaps in vaccine safety data, methodological flaws in studies, or ethical concerns about mandates and informed consent. These critiques are not inherently "antivaccine" but rather reflect a desire for improved accountability, transparency, and scientific rigor.
Hotez fails to engage meaningfully with the underlying issues by conflating these critiques with misinformation. This approach creates an "us vs. them" dynamic, where dissenting voices are marginalized instead of being addressed. Such polarization is detrimental to public health, eroding trust and fueling skepticism.
Engaging with Legitimate Concerns
Public health can benefit from engaging with, rather than suppressing, critique. Legitimate concerns about vaccine safety, efficacy, and policy should be treated as opportunities to improve rather than threats to public health. Constructive engagement requires:
Acknowledging Uncertainties: Public health messaging must openly address gaps in data, limitations of studies, and uncertainties about long-term outcomes. Transparency fosters trust and empowers individuals to make informed decisions.
Encouraging Independent Review: Providing access to raw clinical trial data and safety monitoring reports allows independent researchers to verify findings and address methodological concerns.
Creating Platforms for Dialogue: Public health personnel should establish forums where individuals can raise concerns and have their questions addressed by experts. These platforms should prioritize respectful, evidence-based discussion over dismissal.
Risks of the “Encyclopedia of Vaccine Myths” Approach
Hotez’s proposal for a centralized “encyclopedia of vaccine myths” risks exacerbating the very problem it seeks to solve. By categorizing dissent as myth, this approach could:
Stifle Scientific Progress: Dissent and critique are essential for advancing scientific understanding. Dismissing critique as myth undermines the iterative process of scientific discovery.
Foster Distrust: Labeling concerns as myths without addressing their underlying basis alienates those who feel unheard or dismissed. This approach can backfire, increasing skepticism rather than reducing it.
Obscure Complex Issues: Public health is rarely black and white. Simplifying nuanced concerns into “myths” risks oversimplification, leading to inadequate responses to genuine issues - and will reliably lead to mistrust by the increasingly well-informed public.
Instead of a centralized encyclopedia, a more effective approach would involve real-time engagement with concerns, fostering transparency and building trust. Pediatricians should be required to achieve proficiency in understanding the realities of vaccine risk and the disease burdern of whole-population vaccination in order to continue to practice. Vaccine injury and death risk denial should be discontinued; it is cruel beyond measure, and it is now, clearly, a failed strategy.
Moving Toward Transparency and Dialogue
Public health must adopt a more inclusive and transparent approach to counter misinformation while addressing legitimate concerns. This includes:
Differentiating Critique from Disinformation: Public health messaging should clearly distinguish between valid scientific critiques and factually incorrect claims, addressing each appropriately. Scientific critique should be welcomed.
Acknowledging Historical Mistakes: Public health personnel must learn from past failures, openly acknowledging where safety signals were ignored or mismanaged. They must admit to the bias-inducing procedures they have adopted and help us identify the policies they know are not founded on objective science.
Building Collaborative Platforms: Engaging with vaccine risk-aware individuals, researchers, and advocates can help address concerns constructively and foster a more cooperative public health environment.
Regaining Public Trust
Hotez’s framing of vaccine dissent as disinformation is inaccurate and counterproductive. Public health can regain trust and foster a more informed, collaborative relationship with the public by engaging openly with critique and addressing valid concerns. Suppressing dissent may seem expedient, but it ultimately undermines the transparency and accountability essential for effective public health initiatives and it will make matters far worse.
Broadening Public Health Strategies
Peter Hotez’s narrative focuses narrowly on vaccination as the primary solution to infectious diseases, neglecting the broader social, environmental, and economic factors that significantly influence public health outcomes. While vaccines play an important role in disease prevention, they are not a panacea. Addressing the root causes of disease and integrating vaccines into a comprehensive public health framework is essential for achieving long-term health equity and resilience.
Addressing Root Causes of Disease
Many infectious diseases are driven by systemic issues that vaccines alone cannot resolve. For instance:
Sanitation and Hygiene: Diseases such as cholera and typhoid have been largely eradicated in high-income countries due to improved sanitation, not vaccines. Ensuring access to clean water, waste management, and hygiene education is critical for reducing disease burden globally.
Nutrition and Immune Health: Malnutrition weakens the immune system, making individuals more susceptible to infectious diseases. Addressing food insecurity and promoting balanced diets can significantly enhance immunity and reduce the impact of diseases.
Living Conditions: Overcrowded housing and poor ventilation contribute to the spread of respiratory infections such as tuberculosis and COVID-19. Improving living conditions can mitigate transmission risks.
Focusing solely on vaccination ignores these foundational drivers of health disparities and limits the effectiveness of public health interventions.
Treatments
COVID showed us the lengths to which those who stand to profit from vaccines will go to prevent useful and effective treatment for infectious diseases. Imagine reducing the severity and duration of influenza, measles, varicella, mumps, meningococcus, RSV, hepatitis, diptheria, pertussis, and rubella (among others) with over-the-counter options and clinical treatments in use for decades: glutathione and ozone therapy, iodine, zinc… Physicians should practice medicine first.
Non-Pharmaceutical Interventions
Non-pharmaceutical interventions (NPIs) have proven effective in reducing disease transmission and complementing vaccination efforts. These include:
Improved Ventilation: Upgrading ventilation systems in schools, workplaces, and public spaces can reduce the spread of airborne pathogens.
Hand Hygiene Practices: Public education campaigns on handwashing have been instrumental in reducing gastrointestinal and respiratory infections.
Early Treatment Protocols: Providing access to affordable, evidence-based treatments for early-stage infections can prevent severe disease and reduce healthcare burdens.
While NPIs may not eliminate diseases, they create a multi-layered approach to prevention, enhancing the overall effectiveness of public health strategies.
Using a Holistic Framework
Vaccines may should be come to be seen as an optional part of a larger toolkit for disease prevention, not the sole focus of public health policy. This requires integrating vaccination campaigns with broader initiatives that address determinants of health. For example:
Ensuring the Public Knows Vaccines are Optional with Education: Schools can serve as hubs for health education and information on exemptions to mandates (as required of any ethical system). They can also teach children about hygiene, nutrition, and disease prevention.
Community-Centered Approaches: Engaging local communities in designing and implementing public health interventions ensures that strategies are culturally appropriate and address specific needs.
Holistic Metrics of Success: Public health outcomes should be measured not only by vaccination rates but also by effects of vaccines on disease burden, improved quality of life, and chronic illnesss.
Comprehensive Understanding of Determinants of Health: Physicians and the public should understand that Vitamin D deficiency and selenium deficiency are root cause determinants of individual health, and that integrative, holistic doctors can help define integrative pathways to health (IP2H) that are very different from the relatively more aggressive, paternalistic allopathic medical approach.
Socioeconomic Inequalities and Public Health
Socioeconomic factors play a critical role in health outcomes, yet they are often overlooked in discussions about vaccination. Low-income communities are disproportionately affected by infectious diseases due to limited access to healthcare, poor living conditions, and occupational risks. Addressing these inequities requires:
Accessible Healthcare Services: Ensuring that proper and clean nutrition, and integrative and holistic care and other healthcare resources are available to underserved populations.
Economic Support: Providing financial assistance to individuals who cannot afford private integrative and holistic health solutions.
Policy Reforms: Advocating for policies that reduce barriers to healthcare access, such as expanding Medicaid coverage for integrative approaches to health.
Moving Beyond One-Size-Fits-All Solutions
Hotez’s focus on universal vaccination as the cornerstone of public health overlooks the need for tailored strategies. Different communities face unique challenges and require customized approaches to achieve optimal health outcomes. For instance:
Identifying High-Risk Populations: Every effort should be made to identify individuals and families who cannot tolerate vaccines without suffering increased risk of chronic illness and death.
Adapting to Regional Contexts: Public health strategies must consider regional variations in disease prevalence, infrastructure, and cultural attitudes toward healthcare.
Empowering Local Leaders: Training community leaders to advocate for and implement public health measures can enhance trust and participation. Individuals should seek placement in their local state or county boards of health.
The Role of Public Engagement
Broadening public health strategies requires meaningful engagement with communities to understand their concerns, priorities, and needs. This involves:
Transparent Communication: Providing clear, honest information about the benefits and limitations of various interventions, including vaccines.
Collaborative Decision-Making: Involving community members in designing and evaluating public health programs.
Addressing Misinformation: Countering misinformation with evidence-based education while acknowledging knowledge gaps.
Building Resilience Through Holistic Public Health
The COVID-19 pandemic revealed the vulnerabilities of health systems that rely heavily on vaccines as a singular solution. Building resilience requires a shift toward holistic public health strategies that address the root causes of disease, integrate multiple prevention and treatment modalities, and prioritize health objectivity. By broadening the scope of public health, we can create a more adaptable and sustainable framework for addressing current and future health challenges.
Restoring Trust in Science and Medicine (..and Maybe Public Health)
One of the most significant challenges facing public health today is the erosion of trust in its institutions. The effect has now bled over into widespread mistrust of science and medicine.
This decline can only be exacerbated by the failure to address legitimate concerns, the lack of transparency in decision-making processes, and the coercive nature of some vaccine policies. Peter Hotez’s dismissal of dissent as mere disinformation only deepens these issues, alienating individuals who might otherwise engage constructively. Restoring trust requires a fundamental shift in how public health operates, emphasizing transparency, accountability, and respect for individual autonomy.
Transparency: The Foundation of Trust
Transparency is the cornerstone of trust, yet it is often neglected in public health initiatives. Individuals are more likely to accept and support vaccination when they have access to all relevant information, including risks, benefits, and uncertainties. Current public health messaging, which tends to downplay or dismiss vaccine risks, undermines this trust.
To build transparency, public health personnel must:
Provide Comprehensive Data: Publish raw clinical trial data, safety monitoring reports, and real-world effectiveness studies. These should be accessible to independent researchers and the public for scrutiny.
Acknowledge Uncertainties: Be honest about the limitations of existing studies and the gaps in knowledge, particularly regarding long-term safety and rare adverse events.
Facilitate Open Dialogue: Create forums for public discussion where individuals can ask questions, share concerns, and receive evidence-based responses from experts.
Transparency is about openly sharing what is known and unknown. This approach fosters informed decision-making and strengthens public confidence in public health initiatives.
Accountability: Addressing Past Failures
Public health institutions have a history of ignoring or downplaying safety signals, eroding public confidence. High-profile cases such as the Cutter Incident, Pandemrix-linked narcolepsy, and ongoing concerns about adjuvants like aluminum illustrate the consequences of insufficient accountability. To regain trust, public health must:
Investigate Safety Signals Thoroughly: Commit to rigorous, unbiased investigations of reported adverse events. When signals are identified, they should be addressed transparently, with findings shared publicly and not minimized.
Hold Decision-Makers Accountable: When failures occur, whether due to negligence, conflicts of interest, or poor oversight, there must be consequences. This includes greater oversight of regulatory agencies and removing individuals with vested interests.
Learn from Mistakes: Use past failures as lessons to improve future policies and practices rather than dismissing them as isolated incidents.
Ending Coercion: Respecting Autonomy
Vaccine mandates and social shaming, undermine trust by infringing on personal autonomy. Public health initiatives should focus on fostering voluntary participation through respectful engagement rather than coercion. Key steps include:
Upholding Informed Consent: Ensure that individuals have the information and freedom to make voluntary decisions about vaccination - including their enrollment in long-term safety studies - without fear of penalties or societal pressure.
Providing Alternatives: Develop flexible policies that accommodate diverse risk tolerances and medical conditions, such as allowing exemptions or offering non-invasive testing options for employment or travel.
Empowering Communities: Work with local leaders and organizations to build trust and encourage participation without imposing top-down mandates.
Public health can demonstrate respect for individual rights by prioritizing autonomy while achieving broader health goals.
Fostering Collaboration: Building, Not Burning, Bridges
Public health has increasingly been perceived as adversarial, with dissenters labeled as anti-science or antivaccine. This approach alienates individuals and communities who could be allies in advancing health initiatives. To restore collaboration, public health must:
Engage with Critiques: Treat critiques as opportunities for improvement rather than threats. This requires listening to concerns, addressing valid points, and incorporating feedback into policies.
Collaborate with Diverse Stakeholders: Involve vaccine risk-aware advocates, independent researchers, and community leaders in public health decision-making processes.
Promote Inclusive Policies: Ensure that policies are designed to accommodate diverse perspectives and needs, fostering a sense of shared ownership in public health efforts.
Trust Through Results: Demonstrating Effectiveness and Integrity
Ultimately, trust is earned through results. Public health must not only promise safety and efficacy but also deliver on these promises through robust evidence and transparent practices. This involves:
Active Surveillance Systems: Replace passive systems like VAERS with active monitoring programs that can detect safety signals in real time and that can provide actionable insights.
Continuous Improvement: Adapt policies and practices based on emerging evidence, ensuring that public health programs are effective and responsive to new challenges.
Inclusivity of Approaches: Address barriers to knowledge of integrative approaches to healthcare and ensure that all communities benefit equally from diverse, effective public health initiatives.
A New Vision for Public Health
Restoring trust requires a cultural shift in public health, moving away from paternalistic approaches and toward a model rooted in transparency, accountability, and respect for autonomy. Public health should be seen as a collaborative effort where individuals and communities work together to achieve shared goals using all a
vailable information. By embracing these principles, public health might regain public confidence and create a more resilient, adaptable, and effective system for addressing health challenges.
Citation: Hotez P (2025) It won’t end with COVID: Countering the next phase of American antivaccine activism 2025–29. PLOS Glob Public Health 5(1): e0004020. https://doi.org/10.1371/journal.pgph.0004020



Dr Lyons-Weiler - THIS writing of yours should be in every medical student’s required reading. Brilliant, Spectacular, and so very necessary from. Health Science freedom narrative! And every news media outlet should present this & it should be required reading by every high schooler, college student & in every Drs office. Unfortunately, as long as there are disgusting & pathetic people like Hotez & his falsehoods - we have an uphill battle. But, we are winning. 🔥
Hey Hotez, you genocidal putz: How’s this for anti-vaccine activism (or anti-science(tism) aggression):
* Rushed, guaranteed to succeed, corruptly tested, experimental injection? ✓
* That killed and maimed well-over a thousand people during the severely abbreviated post-trial phase? ✓
* And also caused 23 spontaneous abortions and 75 serious clinical events from 270 expectant mothers during said post-trial? ✓
* Using a highly dangerous mRNA tech that in the past killed every mouse with ADE? ✓
* A tech previously untested on humans, the emergency usage of which upended over a century of vaccine safety and efficacy research? (The following video showcases the grand finale of the FDA SARS-CoV-2 vaccine approval process for 5-11 year olds.) ✓
* For a virus far less deadly than the lockdowns themselves? ✓
* Also less deadly than the flu - which conveniently went AWOL when COVID hit the scene? ✓
* For a (cold) virus they’ve been unable to cure after over a century of trying? ✓
* But somehow all of a sudden, the criminal pharmaceutical companies - notorious for rampant felonious trial fraud - figured it out in less than a year? ✓
* And then went on to manufacture billions of quality assured, safe and effective doses at record speed which were then lawfully distributed by the US military? ✓
* People actually bought into this on a grand scale, and voluntarily injected this poison? ✓
You cannot fix gullible—it has to fix itself. Pain and failure are the best teachers, but no one wants to be their student. The problem with these injections, however, is that you cannot learn from your mistakes if you are dead. If only they would have listened to Fauci:
The best vaccination is to get infected yourself. —Anthony Fauci
More on this and references to all of thr above here: https://tritorch.substack.com/p/the-doormats-of-the-new-world-order