Intelligent Use of Oxygen and Pressure
Understanding the positives and negatives of oxygen in COVID-19 is necessary - and we're not quite there yet.
Right from the start, it was obvious that the effect of SARS-CoV-2 virus on the alveolar sacs in the lungs of COVID-19 patients was different. Unlike most other respiratory viruses, this new virus was capable of infecting lung tissue all the way to the periphery. While this feature, known as Diffuse Alveolar Damage, or DAD, is, for the most part, characteristic of COVID-19 (measles virus also causes DAD), it is not distinguishable from other, non-viral causes of DAD.
Nevertheless, in severe cases, the alveolar phase of COVID-19, patients’ lung tissue is fragile; the damage is extensive, and in the severely affected regions of the lung, the alveolar tissue is thin. There are a large number of other effects, including capillary congestion, platelet-fibrin thrombi (blood clots) in small arterial vessels, along with fibrin, losses in numbers of surfactant-producing cells, and death of pneumocytes (for a few more detailed descriptions see One, Two and Three).
In the US, right from the start, there was a push-pull on the use of ventilators; to some, since COVID-19 was initially described as a type of pneumonia, the use of ventilators per the influenza protocol seemed logical. People with this position were unaware of the paper-thin status of their patients’ lungs; using oxygen and high pressure, intended to save patients, had a twofold effect: first, the physical damage of lung tissue would dramatically reduce patients’ chances of recovery, and second, oxygen itself is, well, highly oxidative. This fact makes the use of high oxygen under pressure precarious for newborns and infants.
Others were more cautious, pointing to the fact that COVID-19 “pneumonia” lacked the hallmarks of influenza pneumonia, and that a lot more was going on at the site of infection than pneumonia.
Image from Alwazeer et al., 2021, Oxid Med & Cell Long.
Eventually, many hospitals learned to ventilate as a method of last resort; oxygen support with positive airway pressure (C-pap and Bi-pap). These, however, can make eating difficult, and physicians still lean toward ventilation too early. In a discussion with Pierre Kory, MD, he reminded me that when severely ill, animals refuse to eat; they reserve their physiologic energies for the battle with the infection or recovery from serious injury, and thus, the while the need to feed a patient eventually becomes reality, the priority should be shutting down the viral replication with early treatments and therapies that are being denied, and helping prevent a runaway immune reaction - the Phase II cytokine storm - with steroids.
Intelligent Use of Oxygen and Pressure
There are other routes to bring oxygen to the patient that does not involve threat to the paper-thin diseased lung tissue in COVID-19 patients. The first worth mentioning is the metabolic maximization of the use of whatever oxygen is available - and a reduction of the dramatically bad effects of excess oxygen. During COVID-19, as in any infection, the rest of the body is fighting to keep up with the accumulation of cellular waste. Lymphocytes show up, ready to clean up the mess of damaged lung tissue, but can find difficult passage to and from the site of injury between blood vessel cells blocked by thrombi, or swollen shut due to inflammation. That’s where glutathione becomes essential.
Glutathione is a sulfur-containing thiol; reduced glutathione (GSH) is considered to be one of the most important scavengers of reactive oxygen species, and its ratio with oxidized glutathione (GSSG) may be used as a marker of oxidative stress. An intracellular antioxidant, it can protect cells against redox damage from the molecular species they must metabolize. Glutathione itself is directly metabolized by dendritic cells, and its balance by regulatory T-cells (Tregs) helps keep immune responses under control. GSH plays an important role in viral infections of the central nervous system and is essential for proper oxygen transport and glucose metabolism in red blood cells. N-acetyl-L-cysteine (NAC) is a pro-GSH supplement, and its effects on the reduction of viral load are well known.
Hyperbaric Oxygen Therapy
The second more intelligent use of oxygen is the use of hyperbaric oxygen therapy (HBOT). A multi-center randomized prospective trial of HBOT found a reduction in the number of days to oxygen normalization. Adoption of HBOT in COVID would reduce the number of days in hospital for people with mild or recovering from severe COVID-19. Prior case studies and non-randomized clinical trials had pointed to the (perhaps obvious) fact that circumventing the damage alveolar surface would lead to a reversal of hypoxia (low blood oxygen levels). Hyperbaric pressure equalizes on both sides of the lung surface, and thus physical damage from positive pressure ventilation can be avoided altogether.
The general clinical utility of HBOT is well known, and the evidence in support of HBOT in medicine just keeps accumulating. It improves brain cellular metabolism in patients with Alzheimer’s disease. It can help improve clinical outcomes of traumatic brain injury - depending on the pressure and gas dose, according to Dr. Paul Harch, the US’s resident senior and leading HBOT guru-at-large.
Also according to Dr. Harch, the mitigation of mitochondrial dysfunction - temporary or chronic - is part of the metabolic and energetic benefits of HBOT. He points out that the world is filled with increasing numbers and abundance of persistent organic pollutants, which have the potential for high toxicity at chronic, low exposures, and the body’s intrinsic detoxification is enhanced during HBOT sessions in ways few other treatments can reach. He points to a review by Dr. Stephan Thom, which presents the evidence of the reduction and reversal of oxidative stress by HBOT. The systemic reversal of hypoxia leads to the shut-down of the production of ROS’s themselves, instead of merely mitigate the symptoms of ROS’s.
Combined Use of GSH Abundance and Hyperbaric Therapies
My friend and colleague, Dr. Ted Fogarty, an acolyte of his mentor Harch, has long been beating the war drums for the grand maximizer, super-exponentiator effects of protecting patients from potential harm from reactive oxidative species (ROS) and the benefits of sufficient oxygen. Hyperbaric pressure, to Ted, is a gift that keeps giving. It drives oxygen to saturation in all tissues, regardless of breathing capacity of patients. But it also allows the body to enjoy an ionic freebie. Ionic gradients across cellular membranes are established - and maintained - at a metabolic cost (expenditure of ATP). This is done via pumps and active transporters embedded in your cell membranes. Ionic gradients are given little thought in medicine, but moving dissolved nutrients, gasses and waste that move with the gradient, while appearing to be passive, are not exactly taking a free ride. The energetics are similar to you spending money from your bank account: the fact that you earned the money, and that it is present and available in your account does not mean it was free money. It’s also similar to dragging a sled uphill: the ride down may seem free, but work must be done to get the sled and its rider up the hill, against the gradient of gravity. Much of cellular energetics and membrane transport are driven by built ionic gradients - against which seemingly passive movement requires the initial expenditure of energy.
Hyperbaric oxygen - and maybe even the pressure itself - changes the stoichiometry of ionic gradients. As Ted puts is “Hyperbarics reverses entropy faster than all in biological systems” - meaning it greases the slide for metabolic processes that would otherwise come a cost.
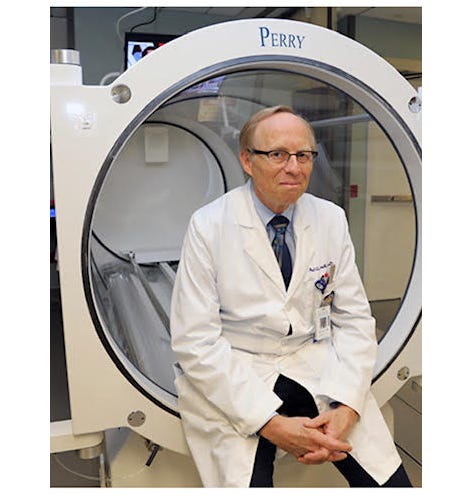
Dr. Paul Harch, Life-Saving HBOT Guru (Click on image for website)
Dr. Fogarty advocating for HBOT Awareness (Click image to visit kxnet.com)
Legacy Medicine Mute on The Intelligent Use of Pressure and Oxygen
Hospitalists and protocolists in the US are largely ignorant of even the adjunctive use of HBOT, yet they decry how filled their hospital beds are. The Pharma-controlled regulatory agencies consider off-label HBOT inquiries as studies on “experimental” treatments; HBOT is established (FDA approved) for many conditions. In spite of the engrained institutional biases, there are currently 13 clinical trials of HBOT use on COVID-19 patients at clinicaltrials.gov from around the world. Sadly, none of them specifically focus on the combined effects of glutathione support and hyperbaric oxygen use.
Some data and studies show promise. Numerous papers have pointed to evidence that HBOT shuts down pro-inflammatory cytokines (e.g., ONE, TWO, THREE). Five patients who faced impending ventilation in Louisiana experienced immediate reversal of the effects of hypoxia due to HBOT therapy.
Regardless, if the concern is only hypoxia, use of HBOT should become routine. The loss of surfactant cells on the gas exchange surface of alveoli alone should be indicative of the need for other routes to oxygenate patients. The added benefits of giving the body a metabolic and energetic break will be discovered (again and again) incidentally, even if not studied overtly - if people pay attention to effect sizes (the measure of benefit) and cite the full literature on hyperbaric physiological and medicinal effects.
FDA needs to be informed by the public that we want GSH support at a minimum - to enhance our glutathione availability - as part of the standard of care - along with the ambulatory treatment protocol of Dr. McCollough and colleagues, and easy-access, inexpensive options including ivermectin - all supported by published research and meta-analyses (see http://c19early.com and https://ivmmeta.com).
Combined therapy trials that test for Dr. Ted and Dr. Harch’s exponential benefits - or even just multiplicative benefits - will provide evidence that will befuddle regulators that tend to be able to focus on 1:1 drug:drug target mechanisms. The answer to the question of “Why people die in the ICU from COVID-19” may or may not be as simple as hypoxia, but instead may require an overhaul of how hypoxia is addressed in hospitals altogether.
Read more on this topic:
Can hyperbaric oxygen safely serve as an anti-inflammatory treatment for COVID-19?






My family experience supports avoiding vents, as 3 of 4 family use Bipap and had mild COVID, while I do not use Bipap and needed 02 to recover. Doc thought I was crazy for saying no to ventilation, while inpatient.
Interesting. Studies have shown NAC significantly reduces the necessity of mechanical ventilation. It would be beneficial to use it earlier in the diseases process where it may help prevent the necessity of hospitalization. Wonder if this is why Amazon pulled it?