Immunosuppression Wars 1.0: VIAIDs
#PathogenicPriming was predicted in April of 2020 and validated by Vojdani et al. Immune Suppression can take many, many forms. AIDS-like T-cell immune suppression is a small part of the story.
This article was inspired by Sofia Karstens who wanted to interview me on immunosuppression. Check out her show with Tony Lyons, The 4th Branch.
There’s something about the SARS-CoV-2 virus proteins and human autoimmunity. For example, Gao et al. (2023) found a lack of coherence between the CD8+ and CD4+ T-cell responses 42 weeks following vaccination with the Pfizer/BioNTech vaccine, but could not explain it.
The number of ways these proteins confound our immune systems is troubling. How many new autoimmune cases will be heading to the doctor’s office for treatment due to vaccination? And what about vaccine-induced acquired immune deficiency (VIAIDS?) Is it real?
We know that during SARS-CoV-2 infection, individuals with prior auto-antibodies - those who already had an autoimmune condition - had worse outcomes. Manry et al. (2022) found that the risk of COVID-19 death is much greater and age-dependent with Type I interferon (IFN) autoantibodies (Manry et al. (2022), known to be associated with a loss of self-tolerance and liver fibrosis (Schinas et al., 2023). Many other studies point to prior autoimmunity as a risk for exposure to SARS-CoV-2 proteins.
Vaccine Recommendations in the Immunocompromised Muddied
Vaccination in the immunocompromised is not a straightforward endeavor. The COVICs study, for example (Haider et al., 2019) found a great range of vaccine responses using standard measures depending on one’s immunocompromised status and vaccination status. Patients who had NOT received an anti-CD20 monoclonal antibody treatment had higher vaccine-induced antibody responses. Patients on HIV drugs, of course are often immunosuppressive. Cancer patients, and patients undergoing transplant are as well. It seems clear that's a problem in an era of COVID-19 and COVID-19 vaccines.
Variation in COVID-19 vaccine response in the immunocompromised tends to be insufficiently studied, and when it is, the conclusion is always “they will just need more boosters”.
Some, such as Marinho (2023) have recognized the additional risk of using live-attenuated COVID-19 vaccines in children who are immunocompromised. The Biden administration just approved another $6Bln in “Private/Public Partnership” for the development of live-attenuated COVID-19 vaccines.
What will this do to people with COVID-19 infection or injection-induced immune deficiencies?
When we induce a vaccine-type, or even an infection-type adaptive immune response, the risk of the virus evolving to evade the immune response in any patient is real. The risk is even higher in immunocompromised patients. For example, seven new haplotypes emerged from a 61-year-old COVID patient who had been treated for follicular lymphoma after six cycles of rituximab and bendamustine. The emergence of variants in highly vaccinated populations points specifically to vaccine failure due to evolution, completely expected in vaccines against mRNA viruses. We have now seen this failure, and the recent “seven boosters” paradigm is proof. Vaccine failure itself involved immunocompromise and immunosuppression. The health effects are increased risk of infection, autoimmunity, and cancer.
Let's unpack that.
New Onset Autoimmunity Diverse and Not Uncommon
New onset autoimmune diseases following COVID-19 vaccination have occurred with sufficient frequency to warrant reporting, including hemophilia (Rawdi & Farsi, 2021), pemphigus (Huang et al., 2022), hepatitis B, immune thrombocytopenia, myocarditis, demyelinating disorder, Guillain-Barré syndrome, immune thrombocytopenia, psoriasis, IgA nephropathy, and systemic lupus erythematosus (Rodríguez et al., 2022).
Chen et al. report occurrences of “Immune thrombotic thrombocytopenia, autoimmune liver diseases, Guillain-Barré syndrome, IgA nephropathy, rheumatoid arthritis, and systemic lupus erythematosus” and others as new-onset following various types of COVID-19 vaccines (Table 2):
A single-center case series study by Alqatari et al. (2023) reported a diversity of new-onset autoimmunity: 7 patients (22.5%) had new-onset vasculitis, 2 cases had IgA vasculitis and 5 cases developed anti-neutrophil cytoplasmic autoantibody (ANCA)-associated vasculitis, 6 cases had neurological diseases (19.3%), 4 cases (12.9%) had new-onset systemic lupus erythematosus (SLE), 3 cases (9.6%) presented with new-onset inflammatory arthritis, and one had Sjogren’s syndrome (3.2%).
Idiopathic cases of Type-I diabetes have also been reported (e.g., Yano et al., 2022), as well as glomerular disease (Meryl et al., 2023) and CD8 T-cell dominant hepatitis (Boettler et al., 2022).
Schinas et al., found vaccine-induced liver damage; see 102 related articles, Pubmed).
Causality: Strong Support from Cross-Study Reproducibility of Dose-Dependence
The average time between vaccination and new-onset disease symptoms varied from 4-7 values following the first dose to 10-14 days after the second dose. For some studies, new onset came on median of 17–22 in those after receiving the third dose. The reproducibility of this variation in risk hints to causality (dose-dependent risk).
In most studies, the highest risk of new-onset autoimmunity followed the second dose, consistent with pathogenic priming.
Many studies could not rule out vaccination as the cause. An Israeli study, for example, found that 85% of disease flares following vaccination could not be attributed to the underlying pathology or condition (Watad et al., 2021).
The vaccine pathway to immunity is clearly not what had been hoped for by vaccine activists. Class-switching appears to be underway in which the immune systems of the vaccinating begin to fail to recognize the endogenously produced spike protein as foreign. This fact, however, has not prevented US FDA from continuing to “approve” COVID-19 boosters. Reports of autoimmunity, serious adverse events, and even deaths in children have not moved the FDA on its position regarding their approval of COVID-19 vaccines. This mindset cannot be explained as resulting from any scientific concern, especially given that FDA has stopped requiring scientific studies for their consideration for approvals, and CDC actually announced they would stop relying on peer-reviewed literature and rely more on non-review papers on preprint servers.
In keeping with the top-down enforced one-sided view of vaccines, most of the studies reporting autoimmunity following vaccination tend to report
Causality is not established (even when conditions for inferring causality are met)
Mechanisms are unclear (even though specific mechanisms are clearly supported by the data
Their studies do not lead to contraindications for anyone, including those at risk of autoimmunity.
Nevertheless, the data fairly well speak for themselves. Rodriguez et al, for example, reported that:
“The first dosage was linked with new-onset events (69.8% vs. 59.3%, P = 0.0100), whereas the second dose was related to relapsing disease (29.5% vs. 59.3%, P = 0.0159). New-onset conditions and relapsing diseases were more common in women (51.5% and 62.9%, respectively; P = 0.0081). The groups were evenly balanced in age. No deaths were recorded after the disease relapsed, while 4.7% of patients with new-onset conditions died (P = 0.0013).”
Mechanisms of VIAIDs (aka Vaccine Immunosuppression)
The cadre of mechanisms at play is crystallizing.
Natural Kill Cell Exhaustion. One of the first modes of pathogenesis recognized by the SARS-CoV-2 spike protein was the exhaustion of NK-cells (Bortolotti et al., 2020). When we cause the exposure of the spike protein to billions, we cause transient suppression of this very important front line of our innate immune system. This necessarily also inhibits other parts of the innate immune response as well as our inherited, generic antibody response.
Immune imprinting (original antigenic sin). When we train the immune system to mount an irrelevant response against an extinct viral type, we not only make the vaccination program futile. We also harm the immune system by limiting the potential immune responses. (See MedicalNewsToday and “SARS-CoV-2 antigen exposure history shapes phenotypes and specificity of memory CD8+ T cells | Nature Immunology”. Immune imprinting in triple-vaccinated healthcare workers was found to profoundly impact immune responses to Omicron (see Immune boosting by B.1.1.529 (Omicron) depends on previous SARS-CoV-2 exposure | Science).
Antibody-Dependent Enhancement (ADE). When we inject the wrong (extinct) type of pathogen protein and individuals are likely to be exposed to newer, updated types, the affinity of the irrelevant antibodies can, for some viruses, make cell entry easier for the newer virus. In addition to the enhancement, the proper adaptive immune response is suppressed. In this way, immune imprinting is built into ADE.
Pathogenic Priming. First proposed by Lyons-Weiler (2020), and validated by Vojdani et al., (2021), pathogenic priming results when we cause multiple exposures to the same viral proteins that contain unsafe epitopes. These are defined as parts of viral proteins that are capable of inducing antibodies that are capable of reacting to the viral protein but also have an affinity for one or more host proteins. The targeted host protein is said to be a molecular mimic of the viral target protein.
Failure of immunotolerance. Recognition of self from non-self is, in my opinion, the most important characteristic of a healthy immune system. When I teach immunology, this is the aspect I stress: Our adaptive immune systems, in fact, all of the cells in our body, are constantly checking themselves to insure they are, in fact, “self”. Some foreign antigen sources are harmless to most people (e.g., peanut antigens); however, likely due to pathogenic priming, some lose tolerance and can become hyperreactive.
We can also lose tolerance of our own innate proteins, which is the very definition of autoimmunity. Loss of tolerance results in autoimmune disorders, such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), type 1 diabetes (T1D) and primary biliary cirrhosis (PBC). (See: Genetic and epigenetic influences on the loss of tolerance in autoimmunity |Nature Magazine)
MHC-1 Suppression. Loss of the MHC-1 pathway can prevent our immune systems from finding and destroying precancerous cells gone rogue. If any of the above mechanisms destroy any component of the MHC-1 pathway, the resulting immunosuppression and loss of self-tolerance to a critical part of our immune system can lead to aggressive, rapidly progressing cancers. Omicron subvariants have shown an increased propensity for MHC-1 suppression (Article), but teasing apart vaccine-induced suppression is challenging unless the vaccination status of patients is also studied.
Moriyama et al (2023) studied MA10 SARS-CoV-2 Omicron variants that had two mutations in the Spike protein (among others). When mice were infected with MA10 and others infected with influenza A, the authors found that compared to the influenza A virus, SARS-CoV-2 MA10 downregulated MHC-I relative to the influenza virus (Fig. 4 A–C).
They wrote:
“Importantly, MHC-I upregulation was completely abrogated in SARS-CoV-2 MA10-infected (S+) lung epithelial cells, suggesting that SARS-CoV-2 viral proteins are strongly inhibiting MHC-I upregulation in a cell-intrinsic manner.”
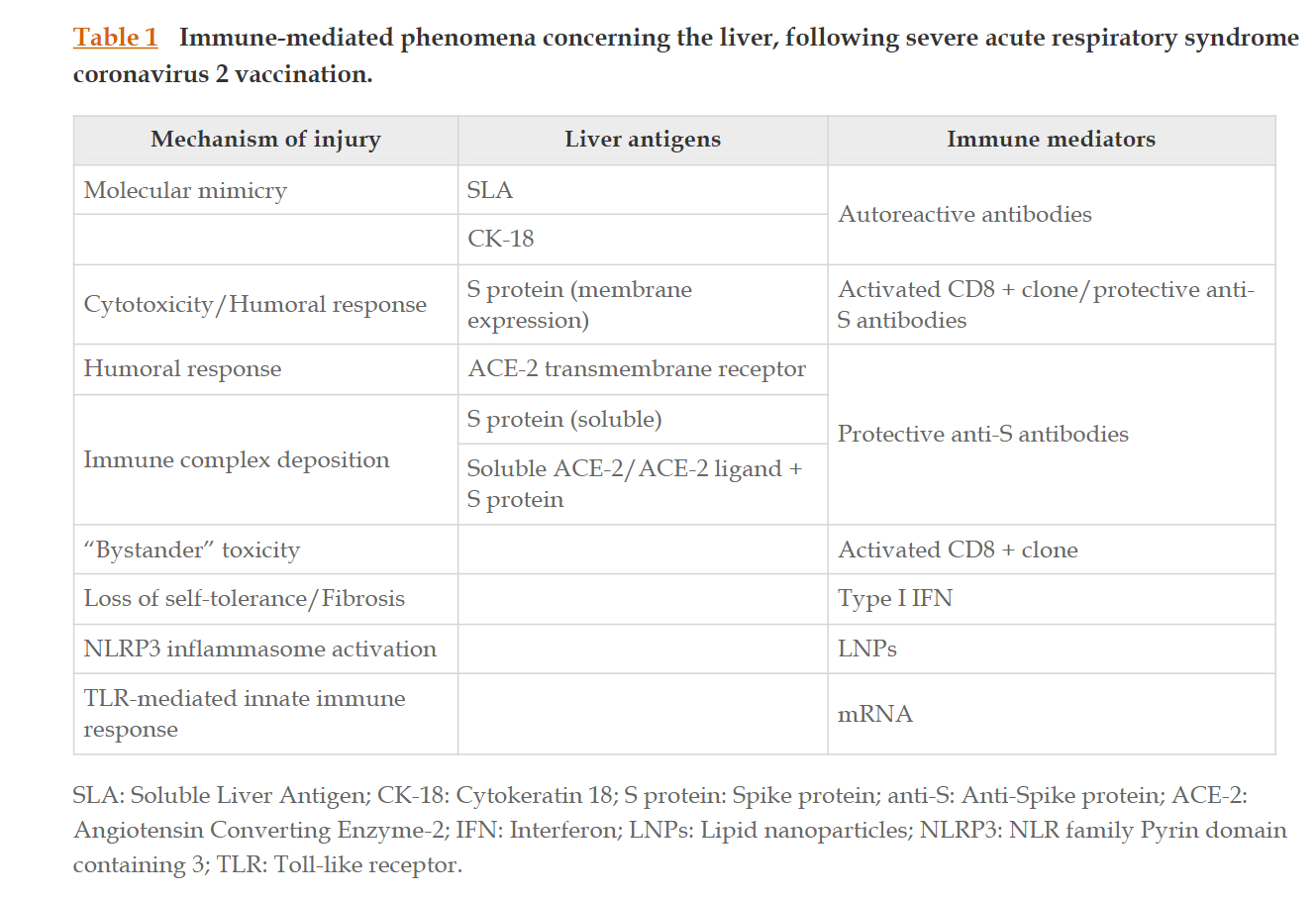
Others exploring mechanisms have focused on particular tissues and organs and similarly cite multiple plausible mechanisms (e.g., Schinas et al., 2023):
“All three most widely distributed severe acute respiratory syndrome coronavirus 2 vaccine formulations, e.g., BNT162b2, mRNA-1273, and ChAdOx1-S, can induce liver injury that may involve immune-mediated pathways and result in an autoimmune hepatitis-like presentation that may require therapeutic intervention in the form of corticosteroid administration. Various mechanisms have been proposed in an attempt to highlight immune checkpoint inhibition and thus establish causality with vaccination. The autoimmune features of such a reaction also prompt an in-depth investigation of the newly employed vaccine technologies. Novel vaccine delivery platforms, e.g., mRNA-containing lipid nanoparticles and adenoviral vectors, contribute to the inflammatory background that leads to an exaggerated immune response, while patterns of molecular mimicry between the spike (S) protein and prominent liver antigens may account for the autoimmune presentation. Immune mediators triggered by vaccination or vaccine ingredients per se, including autoreactive antibodies, cytokines, and cytotoxic T-cell populations, may inflict hepatocellular damage through well-established pathways.”
They provide a table of mechanisms:
In spite of the evidence, some have tried to dismiss autoimmunity from COVID-19 vaccines, but the clinical reality is that physicians see the data that support strong links. So-called “fact-checkers” often funded by vaccine manufacturers or vaccine activists never cite the biomedical research literature on vaccine-induced autoimmunity.
They try to argue (unsuccessfully, in my view) that because the infection can also lead to autoimmunity, there is a risk/benefit to vaccinating. However, I’ve never seen the math - and we won’t because any such comparison ignores joint probabilities of autoimmunity due to dynamics between infections and vaccines. Given the phenomenon of pathogenic priming due to multiple exposures, and the complexities of irrelevant antibodies, the amount of “SARS-CoV-2 related” autoimmunity in a highly vaccinated population must logically be attributed to both the infection rate and the injection rate. Any comparison is a straw man.
It’s worth pointing out that the adenovirus vaccine was identified as a potential risk factor for non-HIV AIDS given a history of increased HIV risk in people receiving modified AV HIV vaccines (See Science article: Could certain COVID-19 vaccines leave people more vulnerable to the AIDS virus? | Science | AAAS). Thus, the adenovirus loaded with spike protein was, out of the box, an acknowledged risk factor for immunosuppression.
References
Alqatari S, Ismail M, Hasan M, Bukhari R, Al Argan R, Alwaheed A, Alkhafaji D, Ahmed SE, Hadhiah K, Alamri T, Nemer A, Albeladi F, Bumurah NN, Sharofna K, Albaggal Z, Alghamdi R, AlSulaiman RS. Emergence of Post COVID-19 Vaccine Autoimmune Diseases: A Single Center Study. Infect Drug Resist. 2023;16:1263-1278
https://doi.org/10.2147/IDR.S394602
Boettler T, Csernalabics B, Salié H, Luxenburger H, Wischer L, Salimi Alizei E, Zoldan K, Krimmel L, Bronsert P, Schwabenland M, Prinz M, Mogler C, Neumann-Haefelin C, Thimme R, Hofmann M, Bengsch B. SARS-CoV-2 vaccination can elicit a CD8 T-cell dominant hepatitis. J Hepatol. 2022 Sep;77(3):653-659. doi: 10.1016/j.jhep.2022.03.040. Epub 2022 Apr 21. PMID: 35461912; PMCID: PMC9021033.
Bortolotti D, Gentili V, Rizzo S, Rotola A, Rizzo R. SARS-CoV-2 Spike 1 Protein Controls Natural Killer Cell Activation via the HLA-E/NKG2A Pathway. Cells. 2020 Aug 26;9(9):1975. doi: 10.3390/cells9091975. PMID: 32859121; PMCID: PMC7563485.
Chen Y, Xu Z, Wang P, Li XM, Shuai ZW, Ye DQ, Pan HF. New-onset autoimmune phenomena post-COVID-19 vaccination. Immunology. 2022 Apr;165(4):386-401. doi: 10.1111/imm.13443. Epub 2022 Jan 7. PMID: 34957554.
Gao, Fei et al. Spheromers reveal robust T cell responses to the Pfizer/BioNTech vaccine and attenuated peripheral CD8+ T cell responses post SARS-CoV-2 infection. Immunity, Volume 56, Issue 4, 864 - 878.e4
https://www.cell.com/immunity/fulltext/S1074-7613(23)00125-5
Haidar G, Agha M, Bilderback A et al. Mellors JW. Prospective Evaluation of Coronavirus Disease 2019 (COVID-19) Vaccine Responses Across a Broad Spectrum of Immunocompromising Conditions: the COVID-19 Vaccination in the Immunocompromised Study (COVICS). Clin Infect Dis. 2022 Aug 24;75(1):e630-e644. doi: 10.1093/cid/ciac103. PMID: 35179197; PMCID: PMC8903515.
https://pubmed.ncbi.nlm.nih.gov/35179197/
Huang X, Liang X, Zhang J, Su H, Chen Y. Pemphigus during the COVID-19 Epidemic: Infection Risk, Vaccine Responses and Management Strategies. J Clin Med. 2022 Jul 8;11(14):3968. doi: 10.3390/jcm11143968. PMID: 35887732; PMCID: PMC9317200.
https://pubmed.ncbi.nlm.nih.gov/35887732/
Manry J, Bastard P, Gervais A… Cobat A et al. The risk of COVID-19 death is much greater and age-dependent with type I IFN autoantibodies. Proc Natl Acad Sci U S A. 2022 May 24;119(21):e2200413119. doi: 10.1073/pnas.2200413119. Epub 2022 May 16. PMID: 35576468; PMCID: PMC9173764.
https://pubmed.ncbi.nlm.nih.gov/35576468/
Marinho AKBB. Vaccination in children with immune-mediated disorders. J Pediatr (Rio J). 2023 Mar-Apr;99 Suppl 1(Suppl 1):S62-S69. doi: 10.1016/j.jped.2022.11.008. Epub 2022 Dec 21. PMID: 36566017; PMCID: PMC10066448.
https://pubmed.ncbi.nlm.nih.gov/36566017/
Meryl et al., COVID-19 Vaccination and New Onset Glomerular Disease: Results from the IRocGN2 International Registry. Kidney360 4(3):p 349-362, March 2023. | DOI: 10.34067/KID.0006832022
https://journals.lww.com/kidney360/Fulltext/2023/03000/COVID_19_Vaccination_and_New_Onset_Glomerular.13.aspx
Minervina AA, Pogorelyy MV, Kirk AM, et al. SARS-CoV-2 antigen exposure history shapes phenotypes and specificity of memory CD8+ T cells. Nat Immunol. 2022 May;23(5):781-790. doi: 10.1038/s41590-022-01184-4. Epub 2022 Apr 5. PMID: 35383307; PMCID: PMC9106845.
https://www.nature.com/articles/s41590-022-01184-4Moriyama M, Lucas C, Monteiro VS; Yale SARS-CoV-2 Genomic Surveillance Initiative; Iwasaki A. Enhanced inhibition of MHC-I expression by SARS-CoV-2 Omicron subvariants. Proc Natl Acad Sci U S A. 2023 Apr 18;120(16):e2221652120. doi: 10.1073/pnas.2221652120. Epub 2023 Apr 10. PMID: 37036977.
https://www.pnas.org/doi/10.1073/pnas.2221652120
Schinas G, Polyzou E, Dimakopoulou V, Tsoupra S, Gogos C, Akinosoglou K. Immune-mediated liver injury following COVID-19 vaccination. World J Virol. 2023 Mar 25;12(2):100-108. doi: 10.5501/wjv.v12.i2.100. PMID: 37033146; PMCID: PMC10075055. https://pubmed.ncbi.nlm.nih.gov/37033146/
Radwi M, Farsi S. A case report of acquired hemophilia following COVID-19 vaccine. J Thromb Haemost. 2021 Jun;19(6):1515-1518. doi: 10.1111/jth.15291. Epub 2021 May 10. PMID: 33783953; PMCID: PMC8250362.
Rodríguez Y, Rojas M, Beltrán S, Polo F, Camacho-Domínguez L, Morales SD, Gersh win ME, Anaya JM. Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review. J Autoimmun. 2022 Oct;132:102898. doi: 10.1016/j.jaut.2022.102898. Epub 2022 Aug 24. PMID: 36041291; PMCID: PMC9399140.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9399140/
Watad A, De Marco G, Mahajna H, Druyan A, Eltity M, Hijazi N, Haddad A, Elias M, Zisman D, Naffaa ME, Brodavka M, Cohen Y, Abu-Much A, Abu Elhija M, Bridgewood C, Langevitz P, McLorinan J, Bragazzi NL, Marzo-Ortega H, Lidar M, Calabrese C, Calabrese L, Vital E, Shoenfeld Y, Amital H, McGonagle D. Immune-Mediated Disease Flares or New-Onset Disease in 27 Subjects Following mRNA/DNA SARS-CoV-2 Vaccination. Vaccines. 2021; 9(5):435. https://doi.org/10.3390/vaccines9050435
https://www.mdpi.com/2076-393X/9/5/435/htm
Vojdani A, Vojdani E, Kharrazian D. Reaction of Human Monoclonal Antibodies to SARS-CoV-2 Proteins With Tissue Antigens: Implications for Autoimmune Diseases. Front Immunol. 2021 Jan 19;11:617089. doi: 10.3389/fimmu.2020.617089. PMID: 33584709; PMCID: PMC7873987. https://pubmed.ncbi.nlm.nih.gov/33584709/
Yano M, Morioka T, Natsuki Y, Sasaki K, Kakutani Y, Ochi A, Yamazaki Y, Shoji T, Emoto M. New-onset Type 1 Diabetes after COVID-19 mRNA Vaccination. Intern Med. 2022 Apr 15;61(8):1197-1200. doi: 10.2169/internalmedicine.9004-21. Epub 2022 Feb 8. PMID: 35135929; PMCID: PMC9107966.
Related
A long-term perspective on immunity to COVID (nature.com)
https://www.nature.com/articles/d41586-021-01557-z
Immunosuppression and SARS-CoV-2 breakthrough infections - The Lancet Rheumatology
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(22)00127-8/fulltext
New Evidence Of Immune Suppression By SARS-CoV-2 (forbes.com)
https://www.forbes.com/sites/williamhaseltine/2021/12/29/new-evidence-of-immune-suppression-by-sars-cov-2/?sh=425ff9e44e76
SARS-CoV-2 proteins are potent suppressors of innate immunity (news-medical.net)
https://www.news-medical.net/news/20210305/SARS-CoV-2-proteins-are-potent-suppressors-of-innate-immunity.aspx
Dendritic cell deficiencies persist seven months after SARS-CoV-2 infection | Cellular & Molecular Immunology (nature.com)
https://www.nature.com/articles/s41423-021-00728-2
Severe COVID-19 patients have impaired plasmacytoid dendritic cell-mediated control of SARS-CoV-2 - PubMed (nih.gov)
https://pubmed.ncbi.nlm.nih.gov/36755036/
Some COVID-19 vaccines could increase HIV risk: researchers (nypost.com)
https://nypost.com/2020/10/20/some-covid-19-vaccines-could-increase-hiv-risk-researchers/





Do people who were "naturally" infected with Covid-19 and then recovered now have the exact same immune system breakdowns occurring as those who were jabbed repeatedly?
Dr. Paul Cottrell and Dr. Ana Mihalcea are claiming that doctors are finding catastrophic breakdowns in blood cells and in plasma as well as extensive tissue damage in both the vaccinated and the unvaccinated.
One would think that picking up a few thousand pathogens through the nasal passages would constitute a qualitative and quantitative difference to the tens of billions or even trillions of mRNA-producing spike proteins that were directly injected into the arm.
IF the jabbed and un-jabbed alike are displaying multiple types of organ failure and much greater propensities of developing cancer (so Cottrell), then this would clearly let Pfizer et al. off the hook because they can easily claim, "See - they're all getting sick even those who have NOT had our products."
Someone should shed light on this growing confusion and conundrum.
- Is pathogenic priming the same thing as molecular mimicry?
- Are autoimmunity mechanisms proper to include in the definition of VIAIDS? AIDS is not considered autoimmune. To me, "immune deficiency" implies reduced ability to fight off disease, where as autoimmunity implies increased ability to cause oneself disease. Perhaps I would append pathogenic priming and failure of immune tolerance to the mechanisms in the Table 1 image and start building a second category of mechanisms relating to autoimmunity and other forms of self-harm. Or perhaps instead, find a better term than VIAIDS to capture all mechanisms of harm at once. But including "AIDS" obviously has an effective ring to it. Some bad suggestions: "VIAIDS+" or "VI-AIDS-AI".
- Don't forget to add IgG4 class switching. I also wonder if class switching could also cause increased tolerance to other coronaviruses?