IgE, Mast Cells, Eosinophils, and Autoimmunity
These important players are underappreciated in autoimmunity. Here's a lyrical essay that might help drive some points home.
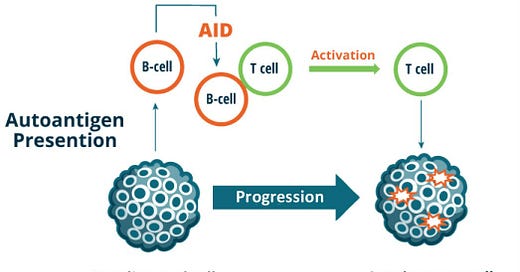
You have likely heard about pathogenic priming leading to molecular mimicry involving self-reactive, or autoreactogenic antibodies. In the intricate tapestry of our immune system, where storms of defense and equilibrium collide, three captivating characters play important, but often underappreciated roles: IgE, mast cells, and eosinophils. Like atmospheric forces shaping weather patterns, these entities hold pivotal roles in immune responses and, intriguingly, their potential interplay with autoimmunity. In this exploration, we shall uncover the essence of IgE, mast cells, and eosinophils, while peering into the enigmatic links between these entities and the triggers of autoimmunity.
IgE – The Sensitivity to Self: IgE, often associated with allergic reactions, possesses an intriguing connection to autoimmunity. Though traditionally seen as orchestrators of allergic responses, IgE’s can also recognize self-antigens, hinting at their involvement in autoimmune conditions. Through mechanisms not yet fully understood, self-reactive IgE antibodies can contribute to the breakdown of immune tolerance, precipitating autoimmune storms that wreak havoc within our bodies. Type I autoimmune (autoallergic) chronic spontaneous urticaria is associated with IgE antibodies against autoantigens, for example, thyroid peroxidase and IL-24.
Mast Cells – The Provocateurs of Self-Perception: Mast cells, like atmospheric provocateurs, may also play a role in autoimmunity. While best known for their contributions to allergic reactions, these versatile cells reside in tissues throughout the body, poised to respond to a wide range of triggers. In the context of autoimmunity, mast cells can be activated by self-antigens, amplifying the immune response and potentially fueling chronic inflammation. Their involvement in autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus hints at their complex interplay with the immune system's delicate balance. Specifically, they are known as effector functions in Th2-skewed allergic and autoimmune inflammation.
Eosinophils – The Storm Troopers of Self-Destruction: Eosinophils, though often associated with allergic responses, also harbor intriguing connections to autoimmunity. These enigmatic cells possess the ability to infiltrate tissues and release cytotoxic proteins. In the realm of autoimmune diseases, eosinophils have been implicated in tissue damage and perpetuation of chronic inflammation. While their precise role in autoimmunity remains an active area of research, their involvement in conditions such as eosinophilic esophagitis and autoimmune vasculitis suggests their potential as players in the autoimmune storm. Eosinophils also should be recognized as playing an important role in Th2-driven inflammation.
The Enigmatic Triggers of Autoimmunity: Autoimmunity, like a complex atmospheric phenomenon, arises from a convergence of triggers. Genetic predisposition, environmental factors, and dysregulation of the immune system all contribute to its onset. In the context of IgE, mast cells, and eosinophils, their potential links to autoimmunity reflect the intricate nature of immune dysregulation. The presence of self-reactive IgE antibodies, aberrant mast cell activation, and eosinophil-mediated tissue damage may all contribute to the development or exacerbation of autoimmune conditions.
In the fascinating complexities of our immune system, IgE, mast cells, and eosinophils cast their intricate shadows upon the realm of autoimmunity. Their roles extend beyond the confines of allergic responses, hinting at potential involvement in the autoimmune storm. While the links between these entities and autoimmunity are still being unraveled, their connections offer new avenues for exploration and understanding. By shedding light on the complex interplay between these cells and the triggers of autoimmunity, we inch closer to deciphering the enigma of immune dysregulation, hoping to calm the tempestuous storms that afflict those with autoimmune conditions.
Lately, the study of IgE, mast cells, eosinophils, and their roles in autoimmunity have become a bit clearer. Research reviews can guide us to a clearer understanding. Hopefully, new research will find ways to harness the interplay of these entities and the rest of the immune system to restore immune harmony and protect those at risk against both external threats and the internal battles that give rise to autoimmune disorders.
For more information on triggers of autoimmunity, please sign up for Autoimmunity and Human Health, meeting this week for the first time on Wednesday at 3:00 PM ET via Zoom. Correction: The original article reported the time as 12:30. Our Microbiome course is at 12:30pm).
Some references
Altrichter S, Fok JS, Jiao Q, Kolkhir P, Pyatilova P, Romero SM, Scheffel J, Siebenhaar F, Steinert C, Terhorst-Molawi D, Xiang YK, Church MK, Maurer M. Total IgE as a Marker for Chronic Spontaneous Urticaria. Allergy Asthma Immunol Res. 2021 Mar;13(2):206-218. doi: 10.4168/aair.2021.13.2.206. PMID: 33474856; PMCID: PMC7840871.
Costela-Ruiz VJ, Illescas-Montes R, Pavón-Martínez R, Ruiz C, Melguizo-Rodríguez L. Role of mast cells in autoimmunity. Life Sci. 2018 Sep 15;209:52-56. doi: 10.1016/j.lfs.2018.07.051. Epub 2018 Jul 29. PMID: 30067942.
Folci M, Ramponi G, Arcari I, Zumbo A, Brunetta E. Eosinophils as Major Player in Type 2 Inflammation: Autoimmunity and Beyond. Adv Exp Med Biol. 2021;1347:197-219. doi: 10.1007/5584_2021_640. PMID: 34031864.



In other words. We are out of our minds to think provoking our immune system with “vaccines” is a good idea for our health. Because there is a whole lot of mechanisms that we don’t understand how they can be provoked to attack self.
A history of rates of autoimmunity would be of interest as well. Sort of like Mark Blaxill’s proof that autism is a man made disaster. One thing the C-19 jabs did, was prove just how much “vaccines” can cause all the injuries we have been witnessing at lower rates in the past.
IgE and EoE are very near and dear to me. My wife has hyper IgE, which damn near killed her when an infection progressed to sepsis. I myself just learned 3 years ago that what I thought was me not chewing my food properly throughout my life was in fact EoE. Now that we are aware of these things we can be aware and be proactive instead of reactive.
What is alarming is how few doctors are aware of it, and if you aren’t an advocate for yourself, they will overlook it as something else. We feel like we are often times educating our doctors on these things.